Breathing difficulty
Shortness of breath; Breathlessness; Difficulty breathing; Dyspnea
Breathing difficulty may involve:
- Difficult breathing
- Uncomfortable breathing
- Feeling like you are not getting enough air
Considerations
There is no standard definition for difficulty breathing. Some people feel breathless with only mild exercise (for example, climbing stairs), even though they don't have a medical condition. Others may have advanced lung disease, but may never feel short of breath. Breathing difficulty is a subjective feeling; only the person feeling it can decide if it is present.
Wheezing is one form of breathing difficulty in which you make a high-pitched sound when you breathe out.

Causes
Shortness of breath has many different causes. For example, heart disease can cause breathlessness if your heart is unable to pump enough blood to supply oxygen to your body. If your brain, muscles, or other body organs do not get enough oxygen, a sense of breathlessness may occur.
Breathing difficulty may also be due to problems with the lungs, airways, or other health problems.
Problems with the lungs:
- Blood clot in the arteries of the lungs (pulmonary embolism)
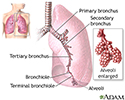
- Swelling and mucus buildup in the smallest air passages in the lungs (bronchiolitis)
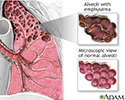
- Chronic obstructive pulmonary disease (COPD), such as chronic bronchitis or emphysema
- Pneumonia
- High blood pressure in the arteries of the lungs (pulmonary hypertension)
- Other lung disease
Problems with the airways leading to the lungs:
- Blockage of the air passages in your nose, mouth, or throat
- Choking on something stuck in the airways
- Swelling around the vocal cords (croup)
- Inflammation of the tissue (epiglottis) that covers the windpipe (epiglottitis)
Problems with the heart:
- Chest pain due to poor blood flow through the blood vessels of the heart (angina)
- Heart attack
- Heart defects from birth (congenital heart disease)
- Heart failure
- Heart rhythm disturbances (arrhythmias)
Other causes:
- Allergies (such as to mold, dander, or pollen)
- High altitudes where there is less oxygen in the air
- Compression of the chest wall
- Dust in the environment
- Emotional distress, such as anxiety
- Hiatal hernia (condition in which part of the stomach extends through an opening of the diaphragm into the chest)
- Obesity
- Panic attacks
- Anemia (low hemoglobin)
- Blood problems (when your blood cells cannot pick up oxygen normally; the disease methemoglobinemia is an example)
- Neuromuscular problems leading to weakness of the breathing muscles
Home Care
Sometimes, mild breathing difficulty may be normal and is not a cause for concern. A very stuffy nose is one example. Strenuous exercise, especially when you do not exercise often, is another example.
If breathing difficulty is new or is getting worse, it may be due to a serious problem. Though many causes are not dangerous and are easily treated, contact your health care provider for any breathing difficulty.
If you are being treated for a long-term problem with your lungs or heart, follow your provider's directions to help with that problem.
When to Contact a Medical Professional
Go to the emergency room or call the local emergency number (such as 911) if:
- Breathing difficulty comes on suddenly or seriously interferes with your breathing and even talking
- Someone completely stops breathing
See your provider if any of the following occur with breathing difficulties:
- Chest discomfort, pain, or pressure. These are symptoms of angina.
- Fever.
- Shortness of breath after only slight activity or while at rest.
- Shortness of breath that wakes you up at night or requires you to sleep propped up to breathe.
- Shortness of breath with simple talking.
- Tightness in the throat or a barking, croupy cough.
- You have breathed in or choked on an object (foreign object aspiration or ingestion).
- Wheezing.
- Significant worsening of baseline shortness of breath.
What to Expect at Your Office Visit
The provider will examine you. You'll be asked about your medical history and symptoms. Questions may include how long you've had difficulty breathing and when it started. You may also be asked if anything worsens it and if you make grunting or wheezing sounds when breathing.
Tests that may be ordered include:
- Blood oxygen saturation (pulse oximetry)
- Blood tests (may include arterial blood gases)
- Chest x-ray
- CT scan of the chest
- Electrocardiogram (ECG)
- Echocardiogram
- Exercise testing
- Lung function tests
If the breathing difficulty is severe, you may need to go to a hospital. You may receive medicines to treat the cause of breathing difficulty.
If your blood oxygen level is very low, you may need oxygen.
References
Braithwaite SA, Wessel AL. Dyspnea. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 21.
Kraft M. Approach to the patient with respiratory disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 77.
Schwartzstein RM, Adams L. Dyspnea. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 36.
Review Date: 5/3/2023