Asbestosis
Pulmonary fibrosis - from asbestos exposure; Interstitial pneumonitis - from asbestos exposure
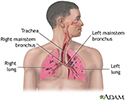
Asbestosis is a lung disease that occurs from breathing in asbestos fibers.
Causes
Breathing in asbestos fibers can cause scar tissue (fibrosis) to form inside the lung. Scarred lung tissue does not expand and contract normally.
How severe the disease is depends on:
- How long the person was exposed to asbestos
- The amount that was breathed in
- The type of fibers breathed in
Often, the symptoms aren't noticed for 20 years or more after the asbestos exposure.
Asbestos fibers were commonly used in construction before 1975.
Asbestos exposure occurs in asbestos mining and milling, construction, fireproofing, and other industries. Household members of asbestos workers can also be exposed from asbestos particles brought home on the worker's clothing.
Other asbestos-related diseases include:
- Pleural plaques
- Malignant mesothelioma (cancer of the pleura, the lining of the lung), which can develop 20 to 40 years after exposure
- Pleural effusion, which is a collection of fluid that develops around the lung a few years after asbestos exposure and is benign
- Lung cancer
These conditions can coexist with asbestosis.
Workers today are less likely to get asbestos-related diseases because of government regulations.
Cigarette smoking increases the risk of developing asbestos-related diseases.
Symptoms
Symptoms may include any of the following:
- Chest pain
- Cough
- Shortness of breath with activity (slowly gets worse over time)
- Tightness in the chest
Possible other symptoms include:
- Clubbing of fingers
- Nail abnormalities
Exams and Tests
Your health care provider will perform a physical exam and ask about the symptoms.
When listening to the chest with a stethoscope, the provider may hear crackling sounds called rales.
These tests may help diagnose the disease:
Pleural plaques in the chest x-ray or CT scan can help diagnose asbestosis and differentiate from other forms of pulmonary fibrosis.
Treatment
There is no cure. Stopping exposure to asbestos is essential. To ease symptoms, drainage and chest percussion can help remove fluids from the lungs.
Your provider may prescribe aerosol medicines to thin lung fluids. People with this condition may need to receive oxygen by mask or by a plastic piece that fits into the nostrils. Certain people may need a lung transplant.
Support Groups
You can ease the stress of this illness by joining a lung support group. Sharing with others who have common experiences and problems can help you not feel alone.
More information and support for people with asbestosis and their families can be found at:
- American Lung Association -- www.lung.org/lung-health-diseases/lung-disease-lookup/asbestosis
- The Asbestos Disease Awareness Organization -- www.asbestosdiseaseawareness.org/
- United States Occupational Safety and Health Administration -- www.osha.gov/asbestos
Outlook (Prognosis)
Outcome depends on the amount of asbestos you were exposed to and how long you were exposed.
People who develop malignant mesothelioma tend to have a poor outcome.
When to Contact a Medical Professional
Contact your provider if you suspect that you have been exposed to asbestos and you have breathing problems. Having asbestosis makes it easier for you to develop lung infections. Talk to your provider about getting the flu, pneumonia, and other vaccines.
If you've been diagnosed with asbestosis, call your provider right away if you develop a cough, shortness of breath, fever, or other signs of a lung infection, especially if you think you have the flu. Since your lungs are already damaged, it's very important to have the infection treated right away. This will prevent breathing problems from becoming severe, as well as further damage to your lungs.
Prevention
In people who have been exposed to asbestos for more than 10 years, screening with a chest x-ray every 3 to 5 years may detect asbestos-related diseases early. Stopping cigarette smoking can greatly reduce the risk of asbestos-related lung cancer.
References
Go LHT, Cohen RA. Pneumoconioses. In: Broaddus VC, Ernst JD, King TE, et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 101.
Tarlo SM. Occupational lung disease. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 87.
Review Date: 5/3/2023
Reviewed By: Denis Hadjiliadis, MD, MHS, Paul F. Harron, Jr. Professor of Medicine, Pulmonary, Allergy, and Critical Care, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.