Reflux nephropathy
Chronic atrophic pyelonephritis; Vesicoureteric reflux; Nephropathy - reflux; Ureteral reflux
Reflux nephropathy is a condition in which the kidneys are damaged by the backward flow of urine into the kidney.
Causes
Urine flows from each kidney through tubes called ureters and into the bladder. When the bladder is full, it squeezes and sends the urine out through the urethra. No urine should flow back into the ureter when the bladder is squeezing. Each ureter has a one-way valve where it enters the bladder that prevents urine from flowing back up the ureter.
But in some people, urine flows back up to the kidney. This is called vesicoureteral reflux.
Over time, the kidneys may be damaged or scarred by this reflux. This is called reflux nephropathy.
Reflux can occur in people whose ureters do not attach properly to the bladder or whose valves do not work well. Children may be born with this problem or may have other birth defects of the urinary system that cause reflux nephropathy.
Reflux nephropathy can occur with other conditions that lead to a blockage of urine flow, including:
- Bladder outlet obstruction, such as an enlarged prostate in men
- Bladder stones
- Neurogenic bladder, which can occur in people with multiple sclerosis, spinal cord injury, diabetes, or other nervous system (neurological) conditions
Reflux nephropathy can also occur from swelling of the ureters after a kidney transplant or from injury to the ureter.
Risk factors for reflux nephropathy include:
- Abnormalities of the urinary tract
- Personal or family history of vesicoureteral reflux
- Repeat urinary tract infections
Symptoms
Some people have no symptoms of reflux nephropathy. The problem may be found when kidney tests are done for other reasons.
If symptoms do occur, they might be similar to those of:
Exams and Tests
Reflux nephropathy is often found when a child is checked for repeated bladder infections. If vesicoureteral reflux is discovered, the child's siblings may also be checked, because reflux can run in families.
Blood pressure may be high, and there may be signs and symptoms of long-term (chronic) kidney disease.
Blood and urine tests will be done, and may include:
- BUN -- blood
- Creatinine -- blood
- Creatinine clearance -- urine and blood
- Urinalysis or 24-hour urine studies
- Urine culture
Imaging tests that may be done include:
- Abdominal CT scan
- Bladder ultrasound
- Intravenous pyelogram (IVP)
- Kidney ultrasound
- Radionuclide cystogram
- Retrograde pyelogram
- Voiding cystourethrogram
Treatment
Vesicoureteral reflux is separated into five different grades. Simple or mild reflux often falls into grade I or II. The severity of the reflux and amount of damage to the kidney help determine treatment.
Simple, uncomplicated vesicoureteral reflux (called primary reflux) can be treated with:
- Antibiotics taken every day to prevent urinary tract infections
- Careful monitoring of kidney function
- Repeated urine cultures
- Yearly ultrasound of the kidneys
Controlling blood pressure is the most important way to slow kidney damage. Your health care provider may prescribe medicines to control high blood pressure. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are often used.
Surgery is usually only used in children who have not responded to medical therapy.
More severe vesicoureteral reflux may need surgery, especially in children who do not respond to medical therapy. Surgery to place the ureter back into the bladder (ureteral reimplantation) can stop reflux nephropathy in some cases.
More severe reflux may need reconstructive surgery. This type of surgery may reduce the number and severity of urinary tract infections.
If needed, people will be treated for chronic kidney disease.
Outlook (Prognosis)
Outcome varies, depending on the severity of the reflux. Some people with reflux nephropathy will not lose kidney function over time, even though their kidneys are damaged. However, kidney damage may be permanent. If only one kidney is involved, the other kidney should keep working normally.
Reflux nephropathy may cause kidney failure in children and adults.
Possible Complications
Complications that may result from this condition or its treatment include:
- Blockage of the ureter after surgery
- Chronic kidney disease
- Chronic or repeat urinary tract infections
- Chronic kidney failure if both kidneys are involved (can progress to end-stage kidney disease)
- Kidney infection
- High blood pressure
- Nephrotic syndrome
- Persistent reflux
- Scarring of the kidneys
When to Contact a Medical Professional
Contact your provider if you:
- Have symptoms of reflux nephropathy
- Have other new symptoms
- Are producing less urine than normal
Prevention
Quickly treating conditions that cause reflux of urine into the kidney may prevent reflux nephropathy.
References
Alexander T, Licht C, Smoyer WE, Rosenblum ND. Diseases of the kidney and upper urinary tract in children. In: Yu ASL, Chertow GM, Luyckx VA, Marsden PA, Skorecki K, Taal MW, eds. Brenner and Rector's The Kidney. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 72.
Mathews R, Damm T, Mattoo TK. Primary vesicoureteral reflux and reflux nephropathy. In: Johnson RJ, Floege J, Tonelli M, eds. Comprehensive Clinical Nephrology. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 62.
Yaqoob MM, Ashman N. Kidney and urinary tract disease. In: Feather A, Randall D, Waterhouse M, eds. Kumar and Clark's Clinical Medicine. 10th ed. Philadelphia, PA: Elsevier; 2021:chap 36.
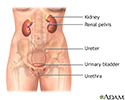
Female urinary tract - illustration
Female urinary tract
illustration
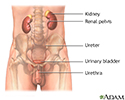
Male urinary tract - illustration
Male urinary tract
illustration
Voiding cystourethrogram - illustration
Voiding cystourethrogram
illustration
Vesicoureteral reflux - illustration
Vesicoureteral reflux
illustration
Review Date: 8/28/2023
Reviewed By: Walead Latif, MD, Nephrologist and Clinical Associate Professor, Rutgers Medical School, Newark, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.