Bladder outlet obstruction
BOO; Lower urinary tract obstruction; Prostatism; Urinary retention - BOO
Bladder outlet obstruction (BOO) is a blockage at the base of the bladder. It reduces or stops the flow of urine into the urethra. The urethra is the tube that carries urine out of the body.
Causes
This condition is common in aging men. It is often caused by enlarged prostate. Bladder stones and bladder cancer are also more commonly seen in men than women. As a man ages, the chances of getting these diseases increase greatly.
Other common causes of BOO include:
- Pelvic tumors (cervix, prostate, uterus, rectum)
- Narrowing of the tube that carries urine out of the body from the bladder (urethra), due to scar tissue or certain birth defects
Less common causes include:
- Cystocele (when the bladder falls into the vagina)
- Foreign objects
- Urethral or pelvic muscle spasms
- Inguinal (groin) hernia
Symptoms
The symptoms of BOO may vary, but can include:
- Abdominal pain
- Continuous feeling of a full bladder
- Frequent urination
- Pain during urination (dysuria)
- Problems starting urination (urinary hesitancy)
- Slow, uneven urine flow, at times being unable to urinate
- Straining to urinate
- Urinary tract infection
- Waking up at night to urinate (nocturia)
Exams and Tests
Your health care provider will ask about your symptoms and medical history. You will undergo a physical exam.
One or more of the following problems may be found:
- Abdominal swelling
- Cystocele (women)
- Enlarged bladder
- Enlarged prostate (men)
Tests may include:
- Blood chemistries to look for signs of kidney damage
- Cystoscopy and retrograde urethrogram (x-ray) to look for narrowing of the urethra
- Tests to determine how fast urine flows out of the body (uroflowmetry)
- Tests to see how much the urine flow is blocked and how well the bladder contracts (urodynamic testing)
- Ultrasound to locate the blockage of urine and find out how well the bladder empties
- Urinalysis to look for blood or signs of infection in the urine
- Urine culture to check for an infection
Treatment
Treatment of BOO depends on its cause. A tube, called a catheter, is inserted into the bladder through the urethra. This is done to relieve the blockage.
Sometimes, a catheter is placed through the belly area into the bladder to drain the bladder. This is called a suprapubic tube.
Most often, you will need surgery for long-term cure of BOO. However, many of the diseases that cause this problem can be treated with medicines. Talk to your provider about possible treatments.
Outlook (Prognosis)
Most causes of BOO can be cured if diagnosed early. However, if the diagnosis or treatment is delayed, this can cause permanent damage to the bladder or kidneys.
When to Contact a Medical Professional
Contact your provider if you have symptoms of BOO.
References
Andersson KE, Wein AJ. Pharmacologic management of lower urinary tract storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 120.
Berney D. Urinary and male genital tracts. In: Cross SS, ed. Underwood's Pathology. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 20.
Boone TB, Stewart JN, Martinez LM. Additional therapies for storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 127.
Capogrosso P, Salonia A, Montorsi F. Evaluation and nonsurgical management of benign prostatic hyperplasia. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 145.
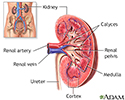
Kidney anatomy - illustration
Kidney anatomy
illustration
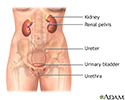
Female urinary tract - illustration
Female urinary tract
illustration
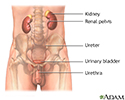
Male urinary tract - illustration
Male urinary tract
illustration
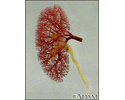
Kidney - blood and urine flow - illustration
Kidney - blood and urine flow
illustration
Review Date: 4/10/2022
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.