Epiglottitis
Supraglottitis
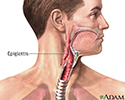
Epiglottitis is inflammation of the epiglottis. This is the tissue-lined cartilage that covers the trachea (windpipe) while swallowing. Epiglottitis can be a life-threatening disease.
Causes
The epiglottis is a stiff, yet flexible tissue (called cartilage) at the back of the tongue. It closes your windpipe (trachea) when you swallow so food does not enter your airway. This helps prevent coughing or choking after swallowing.
In children, epiglottitis is usually caused by the bacteria Haemophilus influenzae (H influenzae) type B. In adults, it is often due to other bacteria such as Streptococcus pneumoniae, or viruses such as herpes simplex virus and varicella-zoster.
Epiglottitis is now very uncommon because the H influenzae type B (Hib) vaccine is given routinely to all children. The disease was once most often seen in children ages 2 through 6. In rare cases, epiglottitis can occur in adults.
Symptoms
Epiglottitis begins with a high fever and sore throat. Other symptoms may include:
- Abnormal breathing sounds (stridor)
- Fever
- Blue skin color (cyanosis)
- Drooling
- Difficulty breathing (the person may need to sit upright and lean slightly forward to breathe)
- Difficulty swallowing
- Voice changes (hoarseness)
The airways can become totally blocked, which can result in cardiac arrest and death.
Exams and Tests
Epiglottitis can be a medical emergency. Seek medical help right away. Do not use anything to press the tongue down to try to look at the throat at home. Doing so may make the condition worse.
The health care provider may examine the voice box (larynx) using a small mirror held against the back of the throat. Or a viewing tube called a laryngoscope may be used. This examination is best done in the operating room or a similar setting where sudden breathing problems can be more easily handled.
Tests that may be done include:
- Blood culture or throat culture
- Complete blood count (CBC)
- Neck x-ray
Treatment
A hospital stay is needed, usually in the intensive care unit (ICU).
Treatment involves methods to help the person breathe, including:
- Breathing tube (intubation)
- Moistened (humidified) oxygen
- A surgical airway, called tracheostomy, as a last resort if other measures fail
Other treatments may include:
- Antibiotics to treat the infection
- Anti-inflammatory medicines, called corticosteroids, to decrease throat swelling
- Fluids given through a vein (by IV)
Outlook (Prognosis)
Epiglottitis can be a life-threatening emergency. With proper treatment, the outcome is usually good.
When to Contact a Medical Professional
Seek immediate medical attention or call 911 or the local emergency number if a person has breathing trouble.
Difficulty breathing is a late, but important sign. Spasm may cause the airways to suddenly close. Or, the airways may become totally blocked. Either of these situations could result in death.
Prevention
The Hib vaccine protects most children from epiglottitis.
The most common bacteria (H influenza type b) that causes epiglottitis is easily spread. If someone in your family is sick from this bacteria, other family members need to be tested and treated.
References
Nayak JL, Weinberg GA. Epiglottitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 63.
Rodrigues KK, Roosevelt GE. Acute inflammatory upper airway obstruction (croup, epiglottitis, laryngitis, and bacterial tracheitis). In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 433.
Epiglottis - illustration
Epiglottis
illustration
Throat anatomy - illustration
Throat anatomy
illustration
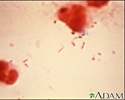
Haemophilus influenzae organism - illustration
Haemophilus influenzae organism
illustration
Haemophilus influenza organism - illustration
Haemophilus influenza organism
illustration
Review Date: 5/2/2024
Reviewed By: Josef Shargorodsky, MD, MPH, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.