Facioscapulohumeral muscular dystrophy
Landouzy-Dejerine muscular dystrophy
Facioscapulohumeral muscular dystrophy is a condition that causes muscle weakness and loss of muscle tissue that gets worse over time.
Causes
Facioscapulohumeral muscular dystrophy is a genetic disease due to a chromosome mutation. It appears in both men and women. It may develop in a child if either parent carries the gene for the disorder. In 10% to 30% of cases, the parents do not carry the gene.
Facioscapulohumeral muscular dystrophy is one of the most common forms of muscle dystrophy affecting 1 in 15,000 to 1 in 20,000 adults in the United States. It affects men and women equally.
Symptoms
Men often have more symptoms than women.
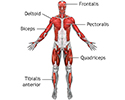
Facioscapulohumeral muscular dystrophy mainly affects the face, shoulder, and upper arm muscles. However, it can also affect muscles around the pelvis, hips, and lower leg.
Symptoms can appear soon after birth (infantile form), but often they do not appear until age 10 to 26 years. However, it is not uncommon for symptoms to appear much later in life. In some cases, symptoms never develop.
Symptoms are most often mild and very slowly become worse. Muscle weakness of the face is common, and may include:
- Eyelid drooping
- Inability to whistle due to weakness of the cheek muscles
- Decreased facial expression due to weakness of facial muscles
- Depressed or angry facial expression
- Difficulty pronouncing words
- Difficulty reaching above the shoulder level
Shoulder muscle weakness causes deformities such as pronounced shoulder blades (scapular winging) and sloping shoulders. The person has difficulty raising their arms because of shoulder and arm muscle weakness.
Weakness of the lower legs is possible as the disorder gets worse. This interferes with ability to play sports because of decreased strength and poor balance. The weakness can be severe enough to interfere with walking. A small percentage of people use a wheelchair.
Chronic pain is present in 50% to 80% of people with this type of muscular dystrophy.
Hearing loss and abnormal heart rhythms may occur, but are rare.
Exams and Tests
A physical exam will show weakness of the face and shoulder muscles as well as scapular winging. Weakness of the back muscles can cause scoliosis, while weakness of the abdominal muscles can be the cause of a sagging belly. High blood pressure may be noted, but is usually mild. An eye exam may show changes in the blood vessels in the back of the eye.
Tests that may be done include:
- Blood creatine kinase levels
- DNA testing
- Electrocardiogram (ECG)
- Electromyography (EMG)
- Fluorescein angiography
- Genetic testing of chromosome 4
- Hearing tests
- Muscle biopsy (may confirm the diagnosis)
- Visual exam
- Cardiac testing
- X-rays of the spine to determine if there is a scoliosis
- Pulmonary function tests
Treatment
Presently, facioscapulohumeral muscular dystrophy remains incurable. Treatments are given to control symptoms and improve quality of life. Activity is encouraged. Inactivity such as bedrest can make the muscle disease worse.
Physical therapy may help maintain muscle strength. Other possible treatments include:
- Occupational therapy to help improve activities of daily living.
- Oral albuterol to increase muscle mass (but not strength).
- Speech therapy.
- Surgery to fix a winged scapula.
- Walking aids and foot support devices if there is ankle weakness.
- BiPAP to help breathing. Oxygen alone should be avoided in patients with a high CO2 (hypercarbia).
- Counseling services (psychiatrist, psychologist, social worker).
Outlook (Prognosis)
Disability is often minor. Lifespan is most often not affected.
Possible Complications
Complications may include:
- Decreased mobility.
- Decreased ability to care for self.
- Deformities of the face and shoulders.
- Hearing loss.
- Vision loss (rare).
- Respiratory insufficiency. (Be sure to talk to your health care provider before having general anesthesia.)
When to Contact a Medical Professional
Contact your provider if symptoms of this condition develop.
Genetic counseling is recommended for couples with a family history of this disease who wish to have children.
References
Bharucha-Goebel DX. Muscular dystrophies. In: Kliegman RM, St Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 627.
Mul K. Facioscapulohumeral muscular dystrophy. Continuum (Minneap Minn). 2022;28(6):1735-1751. PMID: 36537978 pubmed.ncbi.nlm.nih.gov/36537978/.
Muscular Dystrophy Association website. Facioscapulohumeral muscular dystrophy. www.mda.org/disease/facioscapulohumeral-muscular-dystrophy. Accessed March 13, 2024.
Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389.
Warner WC, Sawyer JR. Neuromuscular disorders. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 35.
Review Date: 12/31/2023
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.