Muscular dystrophy
Inherited myopathy; MD
Muscular dystrophy (MD) is a group of inherited disorders that cause muscle weakness and loss of muscle tissue, which get worse over time.
Causes
Inherited conditions are passed down through families. They may become manifest in childhood or adulthood. There are many different types of MD. They include:
- Becker muscular dystrophy
- Duchenne muscular dystrophy
- Emery-Dreifuss muscular dystrophy
- Facioscapulohumeral muscular dystrophy
- Limb-girdle muscular dystrophy
- Oculopharyngeal muscular dystrophy
- Myotonic muscular dystrophy
Symptoms
MD can affect adults, but the more severe forms tend to occur in early childhood.
Symptoms vary among the different types of MD. All of the muscles may be affected. Or, only specific groups of muscles may be affected, such as those around the pelvis, shoulder, or face. The muscle weakness slowly gets worse and symptoms may include:
- Delayed development of muscle motor skills
- Difficulty using one or more muscle groups
- Drooling
- Eyelid drooping (ptosis)
- Frequent falls
- Loss of strength in a muscle or group of muscles as an adult
- Loss in muscle size
- Problems walking (delayed walking)
- Muscle contractures
Intellectual disability is present in some types of MD.
Several types of MD affect only males.
Exams and Tests
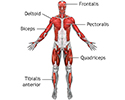
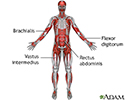
A physical examination and your medical history will help your health care provider determine the type of MD. Specific muscle groups are affected by different types of MD.
The exam may show:
- Weakness of certain muscles
- Abnormally curved spine (scoliosis)
- Joint contractures (clubfoot, claw-hand, or others)
- Low muscle tone (hypotonia)
Some types of MD involve the heart muscle, causing cardiomyopathy or abnormal heart rhythm (arrhythmia).
Often, there is a loss of muscle mass (wasting). This may be hard to see because some types of MD cause a buildup of fat and connective tissue that makes the muscle appear larger. This is called pseudohypertrophy.
A muscle biopsy may be used to confirm the diagnosis. In some cases, a DNA blood test may be all that is needed.
Other tests may include:
- Heart testing -- electrocardiography (ECG)
- Nerve testing -- nerve conduction and electromyography (EMG)
- Urine and blood testing, including creatine phosphokinase (CPK) level
- Genetic testing for some forms of MD
- Muscle biopsy
Treatment
There are no known cures for the various MDs. Recent advances have led to some gene therapies that are promising for the future. The goal of treatment is to control symptoms.
Physical therapy may help maintain muscle strength and function. Leg braces and a wheelchair can improve mobility and self-care. In some cases, surgery on the spine or legs may help improve function.
Corticosteroids taken by mouth are sometimes prescribed to children with certain MDs to keep them walking for as long as possible.
The person should be as active as possible. No activity at all (such as bedrest) can make the disease worse.
Some people with breathing weakness may benefit from devices to assist breathing.
Support Groups
You can ease the stress of illness by joining a support group where members share common experiences and problems.
Outlook (Prognosis)
The severity of disability depends on the type of MD. All types of MD slowly get worse, but how fast this happens varies widely.
Some types of MD, such as Duchenne muscular dystrophy in boys, are associated with a shortened lifespan. Other types cause little disability and people have a normal lifespan.
When to Contact a Medical Professional
Contact your provider if:
- You have symptoms of MD.
- You have a personal or family history of MD and you are planning to have children.
Prevention
Genetic counseling is advised when there is a personal or family history of MD. Women may have no symptoms, but still carry the gene for the disorder. Duchenne muscular dystrophy can be detected with about 95% accuracy by genetic studies done during pregnancy.
References
Manzur AY. Muscular dystrophies. In: Kliegman RM, St. Geme JW, Blum NJ, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 649.
Selcen D. Muscle diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 389.
Review Date: 3/31/2024