Horner syndrome
Oculosympathetic paresis; Horner's syndrome
Horner syndrome is a rare condition that affects the nerves to the eyes and face.
Causes
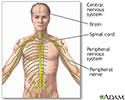
Horner syndrome can be caused by any interruption in a set of nerve fibers that start in the part of the brain called the hypothalamus and travel to the face and eyes. These nerve fibers are involved with sweating, the pupils in your eyes, and the upper and lower eyelid muscles.
Damage of the nerve fibers can result from:
- Injury to the carotid artery, one of the main arteries to the brain
- Injury to nerves at the base of the neck called the brachial plexus or nerve roots
- Migraine or cluster headaches
- Stroke, tumor, or other damage to a part of the brain called the brainstem
- Tumor or infection in the top of the lung, between the lungs, and neck
- Injections or surgery done to interrupt the nerve fibers and relieve pain (sympathectomy)
- Spinal cord injury
In rare cases, Horner syndrome is present at birth. The condition may occur with a lack of color (pigmentation) of the iris (colored part of the eye).
Symptoms
Symptoms of Horner syndrome may include:
- Decreased sweating on the affected side of the face
- Drooping eyelid (ptosis)
- Sinking of the eyeball into the face
- Different sizes of pupils of the eyes (anisocoria) with the affected side pupil being smaller
There may also be other symptoms, depending on the location of the affected nerve fiber. These may include:
- Vertigo (sensation that surroundings are spinning) with nausea and vomiting
- Double vision
- Lack of muscle control and coordination
- Arm pain, weakness and numbness
- One sided neck and ear pain
- Hoarseness
- Hearing loss
- Bladder and bowel difficulty
- Overreaction of the involuntary (autonomic) nervous system to stimulation (hyperreflexia)
Exams and Tests
Your health care provider will perform a physical exam and ask about the symptoms.
An eye exam may show:
- Changes in how the pupil opens or closes
- Constricted pupil
- Eyelid drooping
- Red eye
Depending on the suspected cause, tests may be done, such as:
- Blood tests
- Blood vessel tests of the head (angiogram)
- Chest x-ray or chest CT scan
- MRI or CT scan of the brain or cervical spine
- Spinal tap (lumbar puncture)
- Electromyography and nerve conduction studies if nerve root or brachial plexus injury is suspected
You may need to be referred to a provider who specializes in vision problems related to the nervous system (neuro-ophthalmologist).
Treatment
Treatment depends on the underlying cause of the condition. There is no treatment for Horner syndrome itself. Ptosis is very mild and in rare cases affects vision in Horner syndrome. This can be corrected by cosmetic surgery or treated with eyedrops. Your provider can tell you more.
Outlook (Prognosis)
The outcome depends on whether treatment of the cause is successful.
Possible Complications
There are no direct complications of Horner syndrome itself. But, there may be complications from the disease that caused Horner syndrome or from its treatment.
When to Contact a Medical Professional
Contact your provider if you have symptoms of Horner syndrome.
References
Balcer LJ. Pupillary disorders. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 13.
Tamhankar MA. Eye movement disorders: third, fourth, and sixth nerve palsies and other causes of diplopia and ocular misalignment. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 15.
Thurtell MJ, Rucker JC. Pupillary and eyelid abnormalities. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 17.
Review Date: 6/13/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.