Oral cancer
Cancer - mouth; Mouth cancer; Head and neck cancer - oral; Squamous cell cancer - mouth; Malignant neoplasm - oral; Oropharyngeal cancer - HPV; Carcinoma - mouth
Oral cancer is cancer that starts in the mouth.
Causes
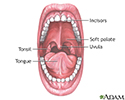
Oral cancer most commonly involves the lips or the tongue. It may also occur on the:
- Cheek lining
- Floor of the mouth
- Gums (gingiva)
- Roof of the mouth (palate)
Most oral cancers are a type called squamous cell carcinoma. These cancers tend to spread quickly.
Smoking and other tobacco use are linked to most cases of oral cancer. Heavy alcohol use also increases the risk for oral cancer.
Human papillomavirus (HPV) infection (the same virus that causes genital warts) account for a larger number of oral cancers than in the past. One type of HPV, type 16 or HPV-16, is much more commonly associated with almost all oral cancers.
Other factors that may increase the risk for oral cancer include:
- Long-term (chronic) rubbing, such as from rough teeth, dentures, or fillings
- Taking medicines (immunosuppressants) that weaken the immune system
- Poor dental and oral hygiene
Some oral cancers begin as a white plaque (leukoplakia) or as a mouth ulcer.
Men develop oral cancer twice as often as women do. It is more common in men older than 40.
Symptoms
Oral cancer can appear as a lump or ulcer in the mouth that may be:
- A deep, hard-edged crack in the tissue
- Pale, dark red, or discolored
- On the tongue, lip, or other area of the mouth
- Painless at first, then a burning sensation or pain when the tumor is more advanced
Other symptoms may include::
- Chewing problems
- Mouth sores that may bleed
- Pain with swallowing
- Speech difficulties
- Swallowing difficulty
- Swollen lymph nodes in the neck
- Tongue problems
- Weight loss
- Difficulty opening the mouth
- Numbness and loosening of teeth
- Bad breath
Exams and Tests
Your health care provider or dentist will examine your mouth area. The exam may show:
- A sore on the lip, tongue, gum, cheeks, or other area of the mouth
- An ulcer or bleeding
A biopsy of the sore or ulcer will be done. This tissue will also be tested for HPV.
CT, MRI, and PET scans may be done to determine if the cancer has spread.
Treatment
Surgery to remove the tumor is recommended if the tumor is small enough.
If the tumor has spread to more tissue or nearby lymph nodes, a larger surgery is done. The amount of tissue and the number of lymph nodes that are removed depend on how far the cancer has spread.
Surgery may be used together with radiation therapy and chemotherapy for larger tumors.
Other treatments may include:
- Targeted therapy, which uses drugs to stop cancer from growing and spreading .
- Immunotherapy, which uses substances made by the body or in a lab to help the immune system work harder or in a more targeted way to fight cancer .
Depending on what type of treatment you require, supportive treatments that may be needed include:
- Speech therapy.
- Therapy to help with chewing and swallowing.
- Learning to eat enough protein and calories to keep your weight up. Ask your provider about liquid food supplements that can help.
- Help with dry mouth.
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
About one half of people with oral cancer will live more than 5 years after they are diagnosed and treated. If the cancer is found early, before it has spread to other tissues, the cure rate ranges from 59% to 94% depending on where the cancer is located. More than half of oral cancers have spread when the cancer is detected. Most have spread to the throat or neck.
Cancers that test positive for HPV appear to respond better to treatment and may have a better outlook. Also, those who smoked for less than 10 years may do better.
People who require larger doses of radiation along with chemotherapy are more likely to have more severe problems with swallowing.
Oral cancers can recur if tobacco or alcohol use is not stopped.
Possible Complications
Complications of oral cancer may include:
- Complications of radiation therapy, including dry mouth and difficulty swallowing
- Disfigurement of the face, head, and neck after surgery
- Other spread (metastasis) of the cancer
When to Contact a Medical Professional
Oral cancer may be discovered when the dentist does a routine cleaning and examination.
Contact your provider if you have a sore in your mouth or lip or a lump in the neck that does not go away within one month. Early diagnosis and treatment of oral cancer greatly increases the chance of survival.
Prevention
Oral cancer may be prevented by:
- Avoiding smoking or other tobacco use
- Having dental problems corrected
- Limiting or avoiding alcohol use
- Visiting the dentist regularly and practicing good oral hygiene
The HPV vaccine recommended for children and young adults targets HPV sub-types most likely to cause oral cancers. They have been shown to prevent most oral HPV infections and 90% of cancers caused by HPV.
References
Kerr AR, Miller CS, Rhodus NL, Stoopler ET, Treister NS. Cancer and oral care of patients with cancer. In: Kerr AR, Miller CS, Rhodus NL, Stoopler ET, Treister NS, eds. Little and Falace's Dental Management of the Medically Compromised Patient. 10th ed. Philadelphia, PA: Elsevier; 2024:chap 26.
National Cancer Institute website. Oropharyngeal cancer treatment (adult) (PDQ) - health professional version. www.cancer.gov/types/head-and-neck/hp/adult/oropharyngeal-treatment-pdq#link/_528. Updated September 5, 2023. Accessed January 16, 2024.
Rettig E, Fakhry C, Gourin CG. Human papillomavirus and the epidemiology of head and neck cancer. In: Flint PW, Haughey BH, Francis HW, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 74.
Wein RO, Weber RS. Malignant neoplasms of the oral cavity. In: Flint PW, Haughey BH, Francis HW, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 91.
Review Date: 12/31/2023
Reviewed By: Josef Shargorodsky, MD, MPH, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.