Valley fever
San Joaquin Valley fever; Coccidioidomycosis; Cocci; Desert rheumatism
Valley fever is an infection that occurs when the spores of the fungus Coccidioides immitis enter your body through the lungs.
Causes
Valley fever is a fungal infection most commonly seen in the desert regions of the southwestern United States, and in Central and South America. You get it by breathing in the fungus from soil. The infection starts in the lungs. It commonly affects people over 60 years of age.
Valley fever may also be called coccidioidomycosis.
Traveling to an area where the fungus is commonly seen raises your risk for this infection. However, you're more likely to develop a serious infection if you live where the fungus is found and have a weakened immune system due to:
- Anti-tumor necrosis factor (TNF) therapy
- Cancer
- Chemotherapy
- Glucocorticoid medicines (prednisone)
- Heart or lung conditions
- HIV/AIDS
- Organ transplant
- Pregnancy (especially the first trimester)
People of Native American, African, or Philippine descent are disproportionately affected.
Symptoms
Most people with valley fever never have symptoms. Others may have cold- or flu-like symptoms or symptoms of pneumonia. If symptoms occur, they typically start 5 to 21 days after exposure to the fungus.
Common symptoms include:
- Ankle, feet, and leg swelling
- Chest pain (can vary from mild to severe)
- Cough, possibly producing blood-tinged phlegm (sputum)
- Fever and night sweats
- Headache
- Joint stiffness and pain or muscle aches
- Loss of appetite
- Painful, red lumps on lower legs (erythema nodosum)
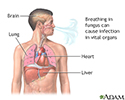
Rarely, the infection spreads from the lungs through the bloodstream to involve the skin, bones, joints, lymph nodes, and central nervous system or other organs. This spread is called disseminated coccidioidomycosis.
People with this more widespread form may become very sick. Symptoms may also include:
- Change in mental status
- Enlarged or draining lymph nodes
- Joint swelling
- More severe lung symptoms
- Neck stiffness
- Sensitivity to light
- Weight loss
Skin lesions of valley fever are often a sign of widespread (disseminated) disease. With more widespread infection, skin sores or lesions are most often seen on the face.
Exams and Tests
The health care provider will perform a physical exam and ask about symptoms and travel history. Tests done for milder forms of this infection include:
- Blood test to check for antibodies to Coccidioides (the fungus that causes Valley fever)
- Chest x-ray
- Sputum culture
- Sputum smear (KOH test)
Tests done for more severe or widespread forms of the infection include:
- Biopsy of the lymph node, lung, or liver
- Bone marrow biopsy
- Bronchoscopy with lavage
- Spinal tap (lumbar puncture) to rule out meningitis
Treatment
If you have a healthy immune system, the disease almost always goes away without treatment. Your provider may suggest bed rest and treatment for flu-like symptoms until your fever disappears.
If you have a weak immune system, you may need antifungal treatment with amphotericin B, fluconazole, or itraconazole. Itraconazole is the drug of choice in people with joint or muscle pain.
Sometimes surgery is needed to remove the infected part of the lung (for chronic or severe disease).
Outlook (Prognosis)
How well you do depends on the form of the disease you have and your overall health.
The outcome in acute disease is likely to be good. With treatment, the outcome is usually also good for chronic or severe disease (although relapses may occur). People with disease that has spread have a high death rate.
Possible Complications
Widespread valley fever may cause:
- Collections of pus in the lung (lung abscess)
- Scarring of the lung
These problems are much more likely if you have a weakened immune system.
When to Contact a Medical Professional
Contact your provider for an appointment if you have symptoms of valley fever or if your condition does not improve with treatment.
Prevention
People with immune problems (such as with HIV/AIDS and those who are on drugs that suppress the immune system) shouldn't go to areas where this fungus is found. If you already live in these areas, other measures that can be taken include:
- Closing windows during dust storms
- Avoiding activities that involve handling soil, such as gardening
Take preventive medicines as prescribed by your provider.
References
Centers for Disease Control and Prevention website. Valley fever (coccidioidomycosis) www.cdc.gov/valley-fever/. Updated April 24, 2024. Accessed June 18, 2024.
Elewski BE, Hughey LC, Hunt KM, Hay RJ. Fungal diseases. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Philadelphia, PA: Elsevier; 2018:chap 77.
Galgiani JN. Coccidioidomycosis (Coccidioides species). In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 265.
Coccidioidomycosis - chest X-ray - illustration
Coccidioidomycosis - chest X-ray
illustration
Pulmonary nodule - front view chest x-ray - illustration
Pulmonary nodule - front view chest x-ray
illustration
Disseminated coccidioidomycosis - illustration
Disseminated coccidioidomycosis
illustration
Fungus - illustration
Fungus
illustration
Coccidioidomycosis - chest X-ray - illustration
Coccidioidomycosis - chest X-ray
illustration
Pulmonary nodule - front view chest x-ray - illustration
Pulmonary nodule - front view chest x-ray
illustration
Disseminated coccidioidomycosis - illustration
Disseminated coccidioidomycosis
illustration
Fungus - illustration
Fungus
illustration
Review Date: 9/10/2022
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.