Whipworm infection
Intestinal parasite - whipworm; Trichuriasis; Round worm - trichuriasis
Whipworm infection is an infection of the large intestine with a type of roundworm.
Causes
Whipworm infection is caused by the roundworm Trichuris trichiura. It is a common infection that mainly affects children.
Children may become infected if they swallow soil contaminated with whipworm eggs. When the eggs hatch inside the body, the whipworm sticks inside the wall of the large intestine.
Whipworm is found throughout the world, especially in countries with warm, humid climates. Some outbreaks have been traced to contaminated vegetables (caused by soil contamination).
Symptoms
Most people who have whipworm infections don't have symptoms. Symptoms mainly occur in children, and range from mild to severe. A severe infection may cause:
- Bloody diarrhea
- Iron-deficiency anemia
- Fecal incontinence (during sleep)
- Rectal prolapse (the rectum comes out of the anus)
Exams and Tests
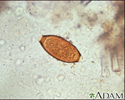
A stool ova and parasites exam reveals the presence of whipworm eggs.
Treatment
The drug albendazole is commonly prescribed when the infection causes symptoms. A different anti-worm medicine may also be prescribed.
Outlook (Prognosis)
Full recovery is expected with treatment.
When to Contact a Medical Professional
Seek medical attention if you or your child develop bloody diarrhea. In addition to whipworm, many other infections and illnesses can cause similar symptoms.
Prevention
Improved facilities for feces disposal have decreased the incidence of whipworm.
Always wash your hands before handling food. Teach your children to wash their hands, too. Thoroughly washing food may also help prevent this condition.
References
Dent AE, Kazura JW. Trichuriasis (Trichuris trichiura). In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 319.
Ince MN, Elliott DE. Intestinal worms. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 114.
Review Date: 12/4/2022
Reviewed By: Jatin M. Vyas, MD, PhD, Associate Professor in Medicine, Harvard Medical School; Associate in Medicine, Division of Infectious Disease, Department of Medicine, Massachusetts General Hospital, Boston, MA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.