Rectal prolapse repair
Rectal prolapse surgery; Anal prolapse surgery
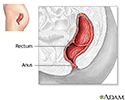
Rectal prolapse repair is surgery to fix a rectal prolapse. This is a condition in which the last part of the intestine (called the rectum) sticks out through the anus.
Description
Rectal prolapse may be partial, involving only the inner lining of the bowel (mucosa). Or, it may be complete, involving the entire wall of the rectum.
For most adults, surgery is used to repair the rectum because there is no other effective treatment.
Children with rectal prolapse do not always need surgery, unless their prolapse does not improve over time. In infants, prolapse often disappears without treatment.
Most surgical procedures for rectal prolapse are done under general anesthesia. For older or sicker people, epidural or spinal anesthesia may be used.
There are three basic types of surgery to repair rectal prolapse. Your surgeon will decide which one is best for you.
For healthy adults, an abdominal procedure has the best chance of success. While you are under general anesthesia, your surgeon makes a cut in the abdomen and removes a portion of the colon. The rectum may be attached (sutured) to the surrounding tissue so it will not slide and fall out through the anus. Sometimes, a soft piece of mesh is wrapped around the rectum to help it stay in place. These procedures can also be done with laparoscopic surgery.
For older adults or those with other medical problems, an approach through the anus (perineal approach) might be less risky. It might also cause less pain and lead to a shorter recovery. But with this approach, the prolapse is more likely to come back (recur).
One of the surgical repairs through the anus involves removing the prolapsed rectum and colon and then suturing the rectum to the surrounding tissues. This procedure can be done under general, epidural, or spinal anesthesia.
Very frail or sick people may need a smaller procedure that reinforces the sphincter muscles. This technique encircles the muscles with a band of soft mesh or a silicone tube. This approach provides only short-term improvement and is rarely used.
Risks
Risks of anesthesia and surgery in general include:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of this surgery include:
- Infection. If a piece of rectum or colon is removed, the bowel needs to be reconnected. In rare cases, this connection can leak, causing infection. More procedures may be needed to treat the infection.
- Constipation is very common, although most people have constipation before the surgery.
- In some people, incontinence (loss of bowel control) can get worse.
- Return of prolapse after abdominal or perineal surgery.
Before the Procedure
During the 2 weeks before your surgery:
- You may be asked to stop taking medicines that make it harder for your blood to clot. Some of these are aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), clopidogrel (Plavix), ticlopidine (Ticlid), and apixaban (Eliquis).
- Ask your health care provider which medicines you should still take on the day of your surgery.
- If you smoke, try to stop. Ask your provider for help.
- Be sure to tell your surgeon if you get sick before your surgery. This includes a cold, flu, herpes flare-up, urinary problems, or any other illness.
The day before your surgery:
- Follow instructions about what you may eat and drink in the days before the operation.
- Follow instructions about when to stop eating or drinking.
- You may be asked to clear out your intestines with a bowel prep. If so, follow those instructions exactly.
On the day of your surgery:
- Take any medicines that your provider told you to take with a small sip of water.
- Be sure to arrive at the hospital on time.
After the Procedure
How long you stay in the hospital depends on the procedure. For open abdominal procedures it may be 5 to 8 days. You will go home sooner if you had laparoscopic surgery. The stay for perineal surgery may be 2 to 3 days.
You should make a complete recovery in 4 to 6 weeks.
Outlook (Prognosis)
The surgery usually works well at repairing the prolapse. Constipation and incontinence can be problems for some people.
References
Galandiuk S, Netz U, Morpurgo E, et al. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 52.
Russ AJ, Delaney CP. Rectal prolapse. In: Fazio the Late VW, Church JM, Delaney CP, Kiran RP, eds. Current Therapy in Colon and Rectal Surgery. 3rd ed. Philadelphia, PA: Elsevier; 2017:chap 22.
Review Date: 3/31/2024
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.