Cosmetic ear surgery
Otoplasty; Ear pinning; Ear surgery - cosmetic; Ear reshaping; Pinnaplasty
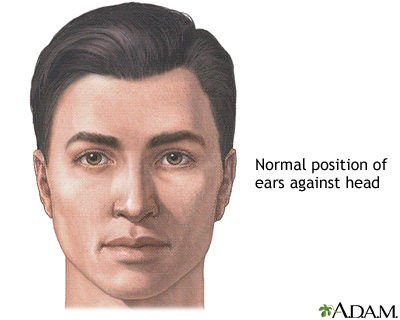
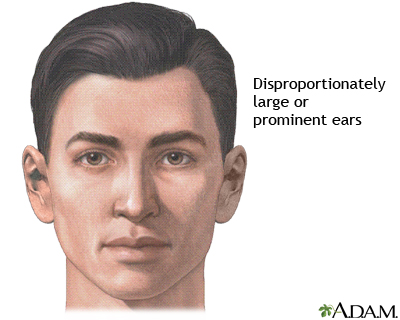
Cosmetic ear surgery is a procedure to improve the appearance of the ear. The most common procedure is to move very large or prominent ears closer to the head.
Description
Cosmetic ear surgery may be done in the surgeon's office, an outpatient clinic, or a hospital. It can be performed under local anesthesia, which numbs the area around the ears. You may also receive medicine to make you relaxed and sleepy. It can also be done under general anesthesia, in which you are asleep and pain-free. This is the preferred method of anesthesia in children. The procedure usually lasts about 2 hours.
During the most common method of cosmetic ear surgery, the surgeon makes a cut in the back of the ear and removes the skin to see the ear cartilage. The cartilage is folded to reshape the ear, bringing it closer to the head. Sometimes the surgeon will cut the cartilage before folding it. Sometimes skin is removed from behind the ear. Stitches are used to close the wound.
Why the Procedure Is Performed
The procedure is often done to reduce self-consciousness or embarrassment of the unusual shape of the ears.
In children, the procedure can be done after they are 5 or 6 years old, when ear growth is almost finished. If the ears are very disfigured (lop ears), the child should have surgery early to avoid possible emotional stress.
Risks
Risks of anesthesia and surgery in general are:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, or infection
Risks of cosmetic ear surgery include:
- Areas of numbness
- Collection of blood (hematoma)
- Infection
- Increased feeling of cold
- Recurrence of the ear deformity
- Keloids and other scars
- Poor results
Before the Procedure
Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including medicines, supplements, or herbs you bought without a prescription
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that reduce the ability of your blood to clot. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
Be sure to follow any other specific instructions from your surgeon.
After the Procedure
The ears are covered with thick bandages with some moderate pressure after surgery. Typically, you can go home after you are awake from the anesthesia.
Any tenderness and discomfort can be controlled with medicine. The ear bandages are usually removed after 2 to 4 days, but may stay on longer. A head wrap or headband needs to be worn for 2 to 3 weeks to help the area heal.
Be sure to contact your surgeon if you have severe ear pain. This can be due to infection of the ear cartilage.
Outlook (Prognosis)
Scars are very light and are hidden in the creases behind the ears.
A second procedure may be needed if the ear sticks out again.
References
Carniol ET, Adamson PA, Gantous A. Otoplasty. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 28.
Thorne CH. Otoplasty and ear reduction. In: Rubin JP, Matarasso A, eds. Plastic Surgery: Volume 2: Aesthetic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2024:chap 23.
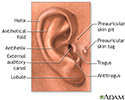
Ear anatomy - illustration
Ear anatomy
illustration
Medical findings based on ear anatomy - illustration
Medical findings based on ear anatomy
illustration
Eardrum repair - series
Presentation
Ear surgery - series
Presentation
Review Date: 12/31/2023
Reviewed By: Tang Ho, MD, Associate Professor, Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology – Head and Neck Surgery, The University of Texas Medical School at Houston, Houston, TX. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.