Breast lump
Breast mass; Breast nodule; Breast tumor
A breast lump is swelling, growth, or mass in the breast.
Breast lumps in both men and women raise concern for breast cancer, even though most lumps are not cancer.
Considerations
Both males and females of all ages have normal breast tissue. This tissue responds to hormone changes. Because of this, lumps can come and go.
Breast lumps may appear at any age:
- Both male and female infants may have breast lumps from their mother's estrogen when they are born. The lump will most often go away on its own as the estrogen clears from the baby's body.
- Young girls often develop "breast buds," which appear just before the beginning of puberty. These bumps may be tender. They are common around age 9, but may happen as early as age 6.
- Teenage boys may develop breast enlargement and lumps because of hormone changes in mid-puberty. Although this may be upsetting to boys, the lumps or growth almost always go away on their own over a period of months.
Causes
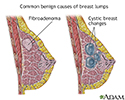
Lumps in a woman are most often either fibroadenomas or cysts, or just normal variations in breast tissue known as fibrocystic changes.
Fibrocystic changes are painful, lumpy breasts. This is a benign condition that does not increase your risk for breast cancer. Symptoms are most often worse right before your menstrual period, and then improve after your period starts.
Fibroadenomas are noncancerous lumps that feel rubbery.
- They move easily inside the breast tissue and are usually not tender. They occur most often during the reproductive years.
- These lumps do not have cancer or become cancerous except in rare cases.
- A health care provider may sometimes suspect a lump is a fibroadenoma based on an exam. Also, an ultrasound and a mammogram can often provide information to determine if a lump looks like a fibroadenoma.
- The only way to be sure, however, is to have a needle biopsy or remove the whole lump.
Cysts are fluid-filled sacs that often feel like soft grapes. These can sometimes be tender, often just before your menstrual period. Ultrasound can determine if a lump is a cyst. It can also reveal whether it is a simple, complicated, or complex cyst.
- Simple cysts are just sacs filled with fluid. They do not need to be removed and may go away on their own. If a simple cyst is growing or causing pain, it can be aspirated.
- A complicated cyst has a little bit of debris in the fluid and can either be watched with ultrasound or the fluid can be drained.
- A complex cyst looks more worrisome on ultrasound. Your provider may recommend either a follow up ultrasound or a needle biopsy. Depending on the results, the cyst may be monitored with ultrasound exams or removed surgically.
Other causes of breast lumps include:
- Breast cancer.
- Injury. Blood may collect and feel like a lump called a hematoma if your breast gets badly bruised. These lumps tend to get better on their own in a few days or weeks. If they do not improve, your provider may have to drain the blood.
- Lipoma. This is a collection of fatty tissue.
- Milk cysts (sacs filled with milk). These cysts can occur with breastfeeding.
- Breast abscess. These typically occur if you are breastfeeding or have recently given birth, but can also occur in women who are not breastfeeding.
Home Care
See your provider if you have any new lumps or breast changes. Ask about your risk factors for breast cancer, and screening and prevention for breast cancer.
When to Contact a Medical Professional
Contact your provider if:
- The skin on your breast appears dimpled or wrinkled (like the peel of an orange).
- You find a new breast lump during self-exam.
- You have bruising on your breast but did not experience any injury.
- You have nipple discharge, especially if it is bloody, clear like water, or pinkish (blood-tinged).
- Your nipple is inverted (turned inward) but normally is not inverted.
Also make contact if:
- You are a woman, age 20 or older, and want guidance on how to perform a breast self-exam.
- You are a woman age 40 or older and have not had a mammogram in the past year for advice about screening for breast cancer.
What to Expect at Your Office Visit
Your provider will get a complete history from you. You will be asked about your factors that may increase your risk for breast cancer. Your provider will perform a thorough breast exam. If you don't know how to perform a breast self-exam, and want to do this, ask your provider to teach you the proper method.
You may be asked medical history questions such as:
- When and how did you first notice the lump?
- Do you have other symptoms such as pain, nipple discharge, or fever?
- Where is the lump located?
- Do you do breast self-exams, and is this lump a recent change?
- Have you had any type of injury to your breast?
- Are you taking any hormones, medicines, or supplements?
Steps your provider may take next include:
- Ordering a mammogram to look for cancer, or a breast ultrasound to see if the lump is solid or a cyst.
- Using a needle to draw fluid out of a cyst. The fluid is usually discarded and does not need to be examined under a microscope.
- Ordering a needle biopsy, which is often done by a radiologist.
How a breast lump is treated depends on the cause.
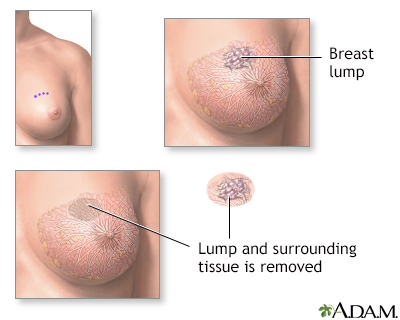
- Solid breast lumps are usually biopsied with a needle by the radiologist. Depending upon the situation, they might be removed with surgery. They can also be monitored over time by your provider.
- Cysts can be drained in your provider's office. If the lump disappears after it is drained, you do not need further treatment. If the lump does not disappear or comes back, you might need to be rechecked with exam and imaging.
- Breast infections are treated with antibiotics. Sometimes a breast abscess needs to be drained with a needle or surgically drained.
- If you are diagnosed with breast cancer, you will discuss your options carefully and thoroughly with your provider.
References
Davidson NE. Breast cancer and benign breast disorders. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 183.
Henry NL, Shah PD, Haider I, Freer PE, et al. Cancer of the breast. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 88.
Klimberg VS, Hunt KK. Diseases of the breast. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. Philadelphia, PA: Elsevier; 2022:chap 35.
Robinson AS, Lee AE. Breast cancer diagnosis and techniques for biopsy. In: Klimberg VS, Gradishar WJ, Bland KI, Korourian S, White J, Copeland EM, eds. Bland and Copeland's The Breast: Comprehensive Management of Benign and Malignant Disorders. 6th ed. Philadelphia, PA: Elsevier; 2024:chap 14.
Vora H, Oseni TO. Breast: benign breast disease. In: Cameron J, ed. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:717-808.
Breast self-exam
Animation
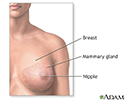
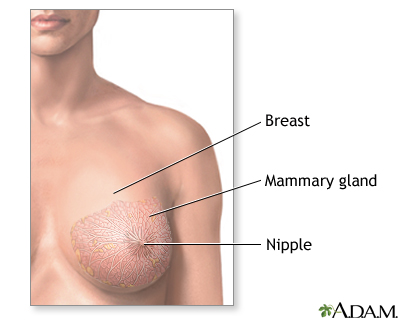
Female Breast - illustration
Female Breast
illustration
Breast lumps - illustration
Breast lumps
illustration
Fibrocystic breast disease - illustration
Fibrocystic breast disease
illustration
Fibroadenoma - illustration
Fibroadenoma
illustration
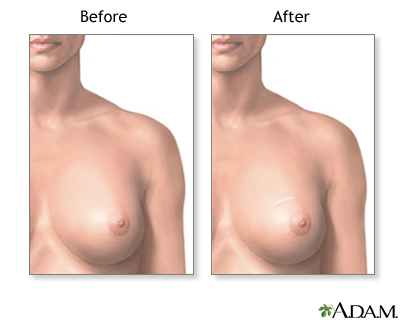
Breast lump removal - series - Normal anatomy
Presentation
Causes of Breast Lumps - illustration
Causes of Breast Lumps
illustration
Core needle biopsy of the breast - illustration
Core needle biopsy of the breast
illustration
Female Breast - illustration
Female Breast
illustration
Breast lumps - illustration
Breast lumps
illustration
Fibrocystic breast disease - illustration
Fibrocystic breast disease
illustration
Fibroadenoma - illustration
Fibroadenoma
illustration
Breast lump removal - series - Normal anatomy
Presentation
Causes of Breast Lumps - illustration
Causes of Breast Lumps
illustration
Core needle biopsy of the breast - illustration
Core needle biopsy of the breast
illustration
Review Date: 11/25/2023
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.