Osmolality urine test
The osmolality urine test measures the concentration of chemicals in urine.
Osmolality in the blood can be measured using a blood test.
A clean-catch urine sample is needed. The clean-catch method is used to prevent germs from the penis or vagina from getting into a urine sample. To collect your urine, your health care provider may give you a special clean-catch kit that contains a cleansing solution and sterile wipes. Follow instructions exactly.
How to Prepare for the Test
Your provider may tell you that you need to limit your fluid intake 12 to 14 hours before the test.
Your provider will ask you to temporarily stop taking any medicines that may affect the test results. Be sure to tell your provider about all the medicines you take, including dextran and sucrose. Do not stop taking any medicine before talking to your provider.
Other things can also affect the test results. Tell your provider if you recently:
- Had any type of anesthesia for an operation.
- Received intravenous dye (contrast medium) for an imaging test such as a CT scan or MRI.
- Used herbs or natural remedies, especially Chinese herbs.
How the Test will Feel
The test involves normal urination. There is no discomfort.
Why the Test is Performed
This test helps check your body's water balance and urine concentration.
Urine osmolality is a more exact measurement of urine concentration than the urine specific gravity test.
Normal Results
Normal values are as follows:
- Random specimen: 50 to 1200 mOsm/kg (50 to 1200 mmol/kg)
- 12 to 14 hour fluid restriction: Greater than 850 mOsm/kg (850 mmol/kg)
Normal value ranges may vary slightly among different laboratories. Some labs use different measurements or test different samples. Talk to your provider about the meaning of your specific test results.
What Abnormal Results Mean
Abnormal results are indicated as follows:
Higher than normal osmolality may indicate:
- Adrenal glands do not produce enough hormones (Addison disease or other types of adrenal insufficiency)
- Glucose (a type of sugar) in the urine
- Heart failure
- High sodium level in the blood
- Loss of body fluids (dehydration)
- Narrowing of the kidney artery (renal artery stenosis)
- Shock
- Syndrome of inappropriate ADH secretion (SIADH)
Lower than normal osmolality may indicate:
- Damage to kidney tubule cells (renal tubular necrosis)
- Diabetes insipidus
- Drinking too much fluid
- Kidney failure
- Low sodium level in the blood
- Severe kidney infection (pyelonephritis)
Risks
There are no risks with this test.
References
Kashkouli A, Berl T, Sands JM. Disorders of water metabolism. In: Johnson RJ, Floege J, Tonelli M, eds. Comprehensive Clinical Nephrology. 7th ed. Philadelphia, PA: Elsevier; 2024:chap 9.
Oh MS, Briefel G, Pincus MR. Evaluation of renal function, water, electrolytes, and acid-base balance. In: McPherson RA, Pincus MR, eds. Henry's Clinical Diagnosis and Management by Laboratory Methods. 24th ed. Philadelphia, PA: Elsevier; 2022:chap 15.
Osmolality test - illustration
Osmolality test
illustration
Female urinary tract - illustration
Female urinary tract
illustration
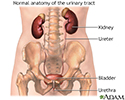
Male urinary tract - illustration
Male urinary tract
illustration
Osmolality urine - series
Presentation
Review Date: 8/20/2023
Reviewed By: Jacob Berman, MD, MPH, Clinical Assistant Professor of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.