Pericardiocentesis
Pericardial tap; Percutaneous pericardiocentesis; Pericarditis - pericardiocentesis; Pericardial effusion - pericardiocentesis
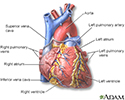
Pericardiocentesis is a procedure that uses a needle to remove fluid from the pericardial sac. This is the tissue that surrounds the heart.
How the Test is Performed
The procedure is most often done in a special procedure room, such as a cardiac catheterization laboratory. It may also be done at a patient's hospital bedside. A health care provider will put an IV into your arm in case fluids or medicines need to be given through a vein. For example, you may be given medicines if your heartbeat slows or your blood pressure drops during the procedure.
The doctor doing the procedure will clean an area just below or next to the breastbone or below the left nipple. Numbing medicine (anesthetic) will be applied to the area.
The doctor will then insert a needle and guide it into tissue that surrounds the heart. Often, echocardiography (ultrasound) is used to help the doctor see the needle and any fluid drainage. An electrocardiogram (ECG) and moving x-ray images (fluoroscopy) may also be used to help with positioning.
Once the needle has reached the correct area, it is removed and replaced with a tube called a catheter. Fluid drains through this tube into containers. Most of the time, the pericardial catheter is left in place so draining may continue for several hours.
Surgical drainage may be needed if the problem is hard to correct or comes back. This is a more invasive procedure in which the pericardium is drained into the chest (pleural) cavity. Alternatively, the fluid may be drained into the peritoneal cavity, but this is less common. This procedure may need to be done under general anesthesia.
How to Prepare for the Test
You may not be able to eat or drink for 6 hours before the test. You must sign a consent form.
How the Test will Feel
You may feel pressure as the needle enters. Some people have chest pain, which may require pain medicine.
Why the Test is Performed
This test may be done to remove and examine fluid that is pressing on the heart. It is most often done to find the cause of a chronic or recurrent pericardial effusion.
It may also be done to treat cardiac tamponade, which is a life-threatening condition.
Normal Results
There is normally a small amount of clear, straw-colored fluid in the pericardial space.
What Abnormal Results Mean
Abnormal findings may indicate the cause of pericardial fluid accumulation, such as:
- Cancer
- Cardiac perforation
- Cardiac trauma
- Congestive heart failure
- Pericarditis
- Renal failure
- Infection
- Rupture of a ventricular aneurysm
Risks
Risks may include:
- Bleeding
- Collapsed lung
- Heart attack
- Infection (pericarditis)
- Irregular heartbeats (arrhythmias)
- Puncture of the heart muscle, coronary artery, lung, liver, or stomach
- Pneumopericardium (air in the pericardial sac)
References
Hoit BD, Oh JK. Pericardial diseases. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 62.
Lewinter MM, Cremer PC, Klein AL. Pericardial diseases. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 86.
Mallemat HA, Tewelde SZ. Pericardiocentesis. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 16.
Review Date: 5/8/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.