Testicular biopsy
Biopsy - testicle
Testicular biopsy is surgery to remove a piece of tissue from the testicles. The tissue is examined under a microscope.
How the Test is Performed
The biopsy can be done in a few ways. The type of biopsy you have depends on the reason for the test. Your health care provider will talk to you about your options.
Open biopsy may be done in the provider's office, a surgical center, or at a hospital. The skin over the testicle is cleaned with a germ-killing (antiseptic) medicine. The area around it is covered with a sterile towel. A local anesthetic is given to numb the area.
A small surgical cut is made through the skin. A small piece of the testicle tissue is removed. The opening in the testicle is closed with a stich. Another stitch closes the cut in the skin. The procedure is repeated for the other testicle if necessary.
Needle biopsy is most often done in the provider's office. The area is cleaned and local anesthesia is used, just as in the open biopsy. A sample of the testicle is taken using a special needle. The procedure does not require a cut in the skin.
Depending on the reason for the test, a needle biopsy may not be possible or recommended.
How to Prepare for the Test
Your provider may tell you not to take aspirin or medicines that contain aspirin for 1 week before the procedure. Always ask your provider before stopping any medicines.
How the Test will Feel
There will be a sting when the anesthetic is given. You should only feel pressure or discomfort similar to a pinprick during the biopsy.
Why the Test is Performed
The test is most often done to find the cause of male infertility. It is done when a semen analysis suggests that there is abnormal sperm and other tests have not found the cause. In some cases, sperm obtained from a testicular biopsy can be used to fertilize a woman's egg in the lab. This process is called in vitro fertilization.
Normal Results
Sperm development appears normal. No cancerous cells are found.
What Abnormal Results Mean
Abnormal results may mean a problem with sperm or hormone function. Biopsy may be able to find the cause of the problem.
In some cases, the sperm development appears normal in the testicle, but semen analysis shows no sperm or reduced sperm. This may indicate a blockage of the tube through which the sperm travel from the testes to the urethra. This blockage can sometimes be repaired with surgery.
Other causes of abnormal results:
- A cyst-like lump filled with fluid and dead sperm cells (spermatocele)
- Orchitis
Your provider will explain and discuss all abnormal results with you.
Risks
There is a slight risk for bleeding or infection. The area may be sore for 2 to 3 days after the biopsy. The scrotum may swell or become discolored. This should clear up within a few days.
Considerations
Your provider may suggest that you wear an athletic supporter for several days after the biopsy. In most cases, you will need to avoid sexual activity for 1 to 2 weeks.
Using a cold pack on and off for the first 24 hours may lessen the swelling and discomfort.
Keep the area dry for several days after the procedure.
Continue to avoid using aspirin or medicines that contain aspirin for 1 week after the procedure.
References
Chiles KA, Schlegel PN. Sperm retrieval. In: Smith JA Jr, Howards SS, Preminger GM, Dmochowski RR, eds. Hinman's Atlas of Urologic Surgery. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 107.
Garibaldi LR, Chemaitilly W. Disorders of pubertal development. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 578.
Niederberger CS, Ohlander SJ, Pagani RL. Male infertility. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 66.
Endocrine glands - illustration
Endocrine glands
illustration
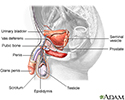
Male reproductive anatomy - illustration
Male reproductive anatomy
illustration
Testicular biopsy - illustration
Testicular biopsy
illustration
Review Date: 1/1/2023
Reviewed By: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.