Health Library
Hip joint replacement
Hip arthroplasty; Total hip replacement; Hip hemiarthroplasty; Arthritis - hip replacement; Osteoarthritis - hip replacement
Hip joint replacement is surgery to replace all or part of the hip joint with a man-made joint. The artificial joint is called a prosthesis.
Images


Presentation

I Would Like to Learn About:
Description
Your hip joint is made up of 2 major parts. One or both parts may be replaced during surgery:
- The hip socket (a part of the pelvic bone called the acetabulum)
- The upper end of the thighbone (called the femoral head)
The new hip that replaces the old one is made up of these parts:
- A socket, which is usually made of strong metal.
- A liner, which fits inside the socket. It is most often plastic. Some surgeons are now trying other materials, such as ceramic or metal. The liner allows the hip to move smoothly.
- A metal or ceramic ball that will replace the round head (top) of your thigh bone.
- A metal stem that is attached to the thigh bone to anchor the joint.
You will not feel any pain during surgery. You will have one of the following types of anesthesia:
- General anesthesia -- This means you will be asleep and unable to feel pain.
- Regional (spinal or epidural) anesthesia -- Medicine is put into your back to make you numb below your waist. You will also get medicine to make you sleepy. And you may get medicine that will make you forget about the procedure, even though you will not be fully asleep.
After you receive anesthesia, your surgeon will make a surgical cut to open up your hip joint. This cut is often over the buttocks or the side of your hip. Then your surgeon will:
- Cut and remove the head of your thigh bone.
- Clean out your hip socket and remove the rest of the cartilage and damaged or arthritic bone.
- Put the new hip socket in place; a liner is then placed in the new socket.
- Insert the metal stem into your thigh bone.
- Place the correct-sized ball for the new joint.
- Secure all of the new parts in place, sometimes with a special cement.
- Repair the muscles and tendons around the new joint.
- Close the surgical wound.
This surgery takes about 1 to 3 hours.
Why the Procedure Is Performed
The most common reason to have this surgery is to relieve arthritis. Severe arthritis pain can limit your activities.
Most of the time, hip joint replacement is done in people age 60 and older. Many people who have this surgery are younger. Younger people who have a hip replaced may put extra stress on the artificial hip. That extra stress can cause it to wear out earlier than in older people. Part or all of the joint may need to be replaced again if that happens.
Your health care provider may recommend a hip replacement for these problems:
- You can't sleep through the night because of hip pain.
- Your hip pain has not gotten better with other treatments.
- Hip pain limits or prevents you from doing your normal activities, such as bathing, preparing meals, doing household chores, and walking.
- You have problems walking that require you to use a cane or walker.
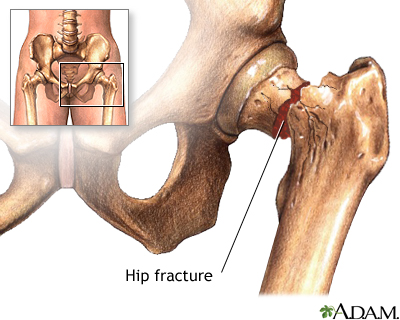
Other reasons for replacing the hip joint are:
- Fractures in the thigh bone. Older adults often have a hip replacement for this reason.
- Hip joint tumors.
Before the Procedure
Always tell your provider what medicines you are taking, even medicine, supplements, or herbs you bought without a prescription. Your provider may also want you to lose weight prior to having surgery.
During the 2 weeks before your surgery:
- Prepare your home to make everyday tasks easier.
- You may be asked to stop taking medicines that make it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), blood thinners such as warfarin (Coumadin), and other medicines.
- You may also need to stop taking medicine that can make you more likely to get an infection. This includes methotrexate, Enbrel, and other medicines that suppress your immune system.
- Ask your surgeon which medicines you should still take on the day of your surgery.
- If you have diabetes, heart disease, or other medical conditions, your surgeon will ask you to see the provider who treats you for these conditions.
- Tell your surgeon if you have been drinking a lot of alcohol, more than 1 or 2 drinks a day.
- If you smoke, you need to stop. Ask your provider or nurse for help. Smoking will slow down wound and bone healing. It has been shown that smokers have worse outcomes after surgery.
- Always let your surgeon know about any cold, flu, fever, herpes breakout, or other illness you have before your surgery.
- You may want to visit a physical therapist to learn some exercises to do before surgery and to practice using crutches or a walker.
- Ask your surgeon to see whether you need to go to a nursing home or rehabilitation facility after surgery. If you do, you should check out these places ahead of time and note your preference.
Practice using a cane, walker, crutches, or wheelchair correctly to:
- Get in and out of the shower
- Go up and down stairs
- Sit down to use the toilet and stand up after using the toilet
- Use the shower chair
On the day of your surgery:
- You will usually be asked not to drink or eat anything for 6 to 12 hours before the procedure.
- Take the medicines your surgeon told you to take with a small sip of water.
Your surgeon will tell you when to arrive at the hospital.
After the Procedure
You will stay in the hospital for 1 to 3 days. During that time, you will recover from your anesthesia and from the surgery itself. You will be asked to start moving and walking as soon as the first day after surgery.
Some people need a short stay in a rehabilitation center after they leave the hospital and before they go home. At a rehab center, you will learn how to safely do your daily activities on your own. Home health services are also available.
Outlook (Prognosis)
Hip replacement surgery results are very often excellent. Most or all of your pain and stiffness should go away.
Some people may have problems with infection, loosening, or even dislocation of the new hip joint.
Over time, the artificial hip joint can loosen. This can happen after as long as 15 to 20 years. You may need a second replacement. An infection can also occur. You should check with your surgeon periodically to ensure your hip is in good condition.
Younger, more active people may wear out parts of their new hip. It may need to be replaced before the artificial hip loosens.
Related Information
ProsthesisIntravenous
Over-the-counter pain relievers
Cuts and puncture wounds
Blood clots
Pulmonary function tests
Community-acquired pneumonia in adults
Urinary catheters
Broken bone
Muscle function loss
Mononeuropathy
Confusion
Osteoarthritis
Rheumatoid arthritis
Hip pain
Osteonecrosis
Bathroom safety for adults
Surgical wound care - open
Preventing falls
Getting your home ready - knee or hip surgery
Hip replacement - discharge
Taking care of your new hip joint
Hip or knee replacement - after - what to ask your doctor
Hip or knee replacement - before - what to ask your doctor
Preventing falls - what to ask your doctor
References
American Academy of Orthopaedic Surgeons website. OrthoInfo. Treatment: total hip replacement. orthoinfo.aaos.org/en/treatment/total-hip-replacement/. Updated June 2020. Accessed August 23, 2023.
Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392(10158):1662-1671. PMID: 30496081 pubmed.ncbi.nlm.nih.gov/30496081/.
Harkess JW, Crockarell JR. Arthroplasty of the hip. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 3.
Rizzo TD. Total hip replacement. In: Frontera WR, Silver JK, Rizzo TD Jr, eds. Essentials of Physical Medicine and Rehabilitation. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 61.
BACK TO TOPReview Date: 8/12/2023
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
 | A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complies with the HONcode standard for trustworthy health information: verify here. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. No warranty of any kind, either expressed or implied, is made as to the accuracy, reliability, timeliness, or correctness of any translations made by a third-party service of the information provided herein into any other language. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
