Fibrous dysplasia
Inflammatory fibrous hyperplasia; Idiopathic fibrous hyperplasia; McCune-Albright syndrome
Fibrous dysplasia is a bone disease that destroys and replaces normal bone with fibrous bone tissue. One or more bones can be affected.
Causes
Fibrous dysplasia usually occurs in childhood. Most people have symptoms by the time they are 30 years old. The disease occurs more often in females.
Fibrous dysplasia is linked to a problem with genes (gene mutation) that control bone-producing cells. The mutation occurs when a baby is developing in the womb. The condition is not passed from parent to child.
Symptoms
Symptoms may include any of the following:
- Bone pain
- Bone sores (lesions)
- Hormone (endocrine gland) problems
- Fractures or bone deformities
- Unusual skin color (pigmentation), which occurs with McCune-Albright syndrome
The bone lesions may stop when the child reaches puberty.
Exams and Tests
Your health care provider will perform a physical examination. X-rays of bones are taken. An MRI may be recommended.
Treatment
There is no cure for fibrous dysplasia. Bone fractures or deformities are treated as needed. Hormone problems will need to be treated.
Outlook (Prognosis)
The outlook depends on the severity of the condition and the symptoms that occur.
Possible Complications
Depending on the bones that are affected, health problems that may result include:
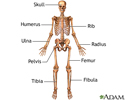
- If skull bone is affected, there can be vision or hearing loss
- If a leg bone is affected, there can be difficulty walking and joint problems such as arthritis
When to Contact a Medical Professional
Contact your provider if your child has symptoms of this condition, such as repeated bone fractures and unexplained bone deformity.
Specialists in orthopedics, endocrinology, and genetics may be involved in your child's diagnosis and care.
Prevention
There is no known way to prevent fibrous dysplasia. Treatment aims to prevent complications, such as recurrent bone fractures, to help make the condition less severe.
References
Nadol JB, Quesnel AM. Otologic manifestations of systemic disease. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 151.
Nicolai P, Mattavelli D, Castlenuovo P. Benign tumors of the sinonasal tract. In: Flint PW, Francis HW, Haughey BH, et al, eds. Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 50.
Shiflett JM, Caroll BW. Skull lesions in children. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 245.
Toy PC, Heck RK. Benign bone tumors and nonneoplastic conditions simulating bone tumors. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 25.
Review Date: 11/6/2023
Reviewed By: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.