Intestinal obstruction repair
Repair of volvulus; Intestinal volvulus - repair; Bowel obstruction - repair
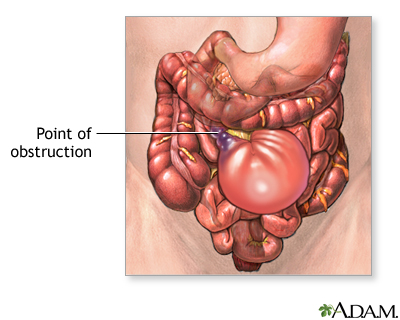
Intestinal obstruction repair is surgery to relieve a bowel obstruction. A bowel obstruction occurs when the contents of the intestines cannot pass through and exit the body. A complete obstruction is a surgical emergency.
Description
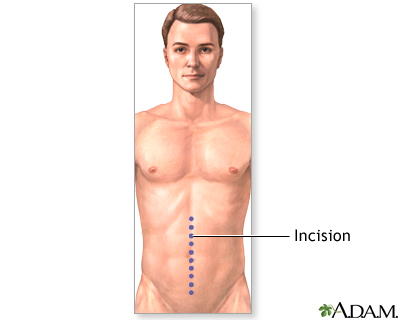
Intestinal obstruction repair is done while you are under general anesthesia. This means you are asleep and do not feel pain.
Your surgeon makes a cut in your belly to see your intestines. Sometimes, the surgery can be done using a laparoscope, which means smaller cuts are used.
Your surgeon locates the area of your intestine (bowel) that is blocked and unblocks it.
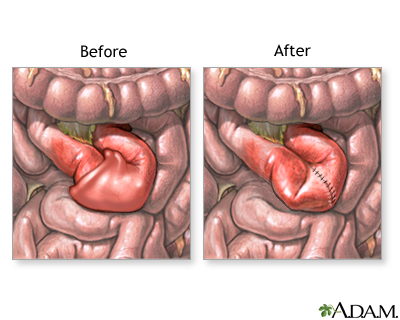
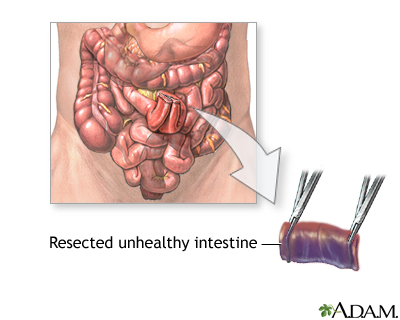
Any damaged parts of your bowel will be repaired or removed. This procedure is called bowel resection. If a section is removed, the healthy ends will be reconnected with stitches or staples. Sometimes, when part of the intestine is removed, the ends cannot be reconnected. If this happens, your surgeon will bring one end out through an opening in the abdominal wall. This may be done using a colostomy or ileostomy.
Why the Procedure Is Performed
This procedure is done to relieve a blockage in your intestine. A blockage that lasts for a long time can reduce or block blood flow to the area. This can cause the bowel to die.
Risks
Risks of anesthesia and surgery in general include:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of this procedure:
- Bowel obstruction after surgery
- Damage to nearby organs in the body
- Formation of scar tissue (adhesions)
- More scar tissue forming in your belly and causing a blockage of your intestines in the future
- Opening of the edges of your intestines that are sewn together (anastomotic leak), which may cause life-threatening problems
- Problems with the colostomy or ileostomy
- Temporary paralysis (freezing up) of the bowel (paralytic ileus)
After the Procedure
How long it takes to recover depends on your overall health and the type of operation.
Outlook (Prognosis)
The outcome is usually good if the obstruction is treated before bowel blood flow is affected.
People who have had many abdominal surgeries may form scar tissue. They are more likely to have bowel obstructions in the future.
References
Galandiuk S, Netz U, Morpurgo E, et al. Colon and rectum. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 52.
Mustain WC, Turnage RH. Intestinal obstruction. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology/Diagnosis/Management. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 123.
Senagore AJ, Rojas-Khalil Y. Management of large bowel obstruction. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 14th ed. Philadelphia, PA: Elsevier; 2023:209-214.
Before and after small intestine anastomosis - illustration
Before and after small intestine anastomosis
illustration
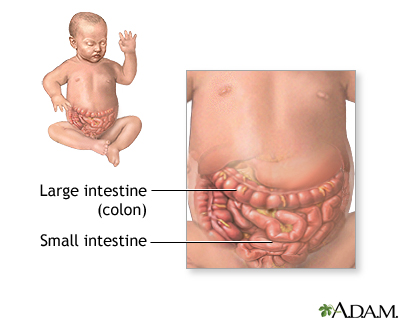
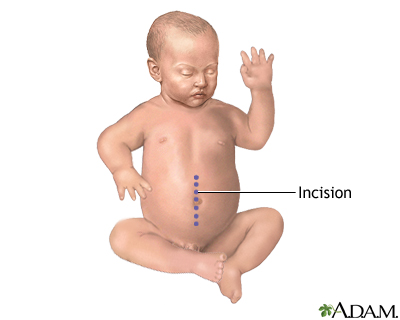
Intestinal obstruction (pediatric) - series
Presentation
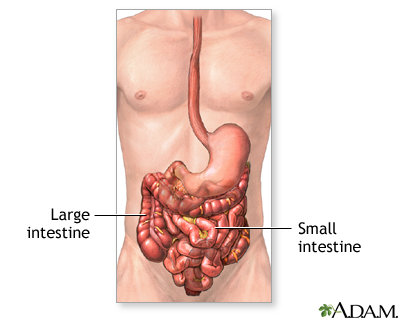
Intestinal obstruction repair - series
Presentation
Review Date: 3/31/2024
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.