Thyroid gland removal
Total thyroidectomy; Partial thyroidectomy; Thyroidectomy; Subtotal thyroidectomy; Thyroid cancer - thyroidectomy; Papillary cancer - thyroidectomy; Goiter - thyroidectomy; Thyroid nodules - thyroidectomy
Thyroid gland removal is surgery to remove all or part of the thyroid gland. The thyroid gland is a butterfly-shaped gland located inside the front of the lower neck.
The thyroid gland is part of the hormone (endocrine) system. It helps your body regulate your metabolism.
Description
Depending on the reason you are having your thyroid gland removed, the type of thyroidectomy you have will be either a:
- Total thyroidectomy, which removes the entire gland
- Subtotal or partial thyroidectomy, which removes part of the thyroid gland
You will have general anesthesia (asleep and pain-free) for this surgery. In rare cases, the surgery is done with local anesthesia and medicine to relax you. You will be awake, but pain-free.
During the surgery:
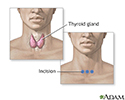
- The surgeon makes a horizontal cut in the front of your lower neck just above the collar bones.
- All or part of the gland is removed through the cut.
- The surgeon is careful not to damage the blood vessels and nerves in your neck.
- A small tube (catheter) may be placed into the area to help drain blood and other fluids that build up. The drain will be removed in 1 or 2 days.
- The cuts are closed with sutures (stitches).
Surgery to remove your whole thyroid may take 2 to 3 hours. It may take less time if only part of the thyroid is removed.
Newer techniques that require a smaller incision near the thyroid or at other locations and which involve the use of endoscopy have been developed.
Why the Procedure Is Performed
Your health care provider may recommend thyroid removal if you have any of the following:
- A small thyroid growth (nodule or cyst)
- A thyroid gland that is so overactive it is dangerous (thyrotoxicosis)
- Cancer of the thyroid
- Noncancerous (benign) tumors of the thyroid that are causing symptoms
- Thyroid swelling (nontoxic goiter) that makes it hard for you to breathe or swallow
You may also have surgery if you have an overactive thyroid gland and do not want to have radioactive iodine treatment, or you cannot be treated with antithyroid medicines.
Risks
Risks of anesthesia and surgery in general include:
- Reactions to medicines
- Breathing problems
- Bleeding, blood clots, infection
Risks of thyroidectomy include:
- Injury to the nerves to your vocal cords and larynx.
- Bleeding and possible airway obstruction.
- A sharp rise in thyroid hormone levels (only around the time of surgery).
- Injury to the parathyroid glands (small glands near the thyroid) or to their blood supply. This can cause a temporary low level of calcium in your blood (hypocalcemia).
- Too much thyroid hormone (thyroid storm). If you have an overactive thyroid gland, you will be treated with medicine.
Before the Procedure
Tell your surgeon or nurse if:
- You are or could be pregnant
- You are taking any medicines, including drugs, supplements, or herbs you bought without a prescription
During the weeks before your surgery:
- You may need to have tests that show exactly where the abnormal thyroid growth is located. This will help your surgeon find the growth during surgery. You may have a CT scan, ultrasound, or other imaging tests.
- Your provider may also do a fine needle aspiration to find out if the growth is noncancerous or cancerous. Before surgery, your vocal cord function may be checked.
- You may also need thyroid medicine or iodine treatments 1 to 2 weeks before your surgery.
During the week before your surgery:
- You may be asked to temporarily stop taking medicines that keep your blood from clotting. These medicines are called blood thinners. This includes over-the-counter medicines and supplements such as aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve, Naprosyn), and vitamin E. Many prescription medicines are also blood thinners.
- Ask your surgeon which medicines you should still take on the day of surgery.
- Fill any prescriptions for pain medicine and calcium you will need after surgery.
- If you smoke, try to stop. Ask your provider for help.
On the day of surgery:
- Follow instructions about when to stop eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the Procedure
You will probably go home the day of or the day after surgery. In rare cases, you may need to spend up to 3 days in the hospital. You must be able to swallow liquids before you can go home.
Your surgeon may check the calcium level in your blood after surgery. This is done more often when the whole thyroid gland is removed.
You may have some pain after surgery. Ask your surgeon for instructions on how to take pain medicines after you go home.
It should take about 4 to 6 weeks for you to fully recover.
Follow any instructions for taking care of yourself after you go home.
Outlook (Prognosis)
Outcome of this surgery is usually excellent. Most people need to take thyroid hormone pills (thyroid hormone replacement) for the rest of their lives when the whole gland is removed.
References
Ferris RL, Turner MT. Minimally invasive video-assisted thyroidectomy. In: Myers EN, Snyderman CH, eds. Operative Otolaryngology Head and Neck Surgery. 3rd ed. Philadelphia, PA: Elsevier; 2018:chap 79.
Pace-Asciak P, Russell JO, Razavi CR, et al. Surgical management of thyroid disease. In: Robertson RP, Giudice LC, Grosman AB, eds. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 82.
Patel KN, Yip L, Lubitz CC, et al. Executive summary of the American Association of Endocrine Surgeons guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020;271(3):399-410. PMID: 32079828 pubmed.ncbi.nlm.nih.gov/32079828/.
Suh I, Sosa JA. Thyroid. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 37.
Child thyroid anatomy - illustration
Child thyroid anatomy
illustration
Thyroidectomy - Series
Presentation
Incision for thyroid gland surgery - illustration
Incision for thyroid gland surgery
illustration
Review Date: 3/31/2024
Reviewed By: Debra G. Wechter, MD, FACS, General Surgery Practice Specializing in Breast Cancer, Virginia Mason Medical Center, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.