Chronic inflammatory demyelinating polyneuropathy
Chronic inflammatory demyelinating polyradiculoneuropathy; Polyneuropathy - chronic inflammatory; CIDP; Chronic inflammatory polyneuropathy; Guillain-Barré - CIDP
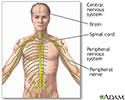
Chronic inflammatory demyelinating polyneuropathy (CIDP) is a disorder that involves nerve swelling and irritation (inflammation) that leads to a loss of strength or sensation.
Causes
CIDP is one cause of damage to nerves outside the brain or spinal cord (peripheral neuropathy). Polyneuropathy means several nerves are involved. CIDP often affects both sides of the body.
CIDP is caused by an abnormal immune response. CIDP occurs when the immune system attacks the myelin cover of the nerves. For this reason, CIDP is thought to be an autoimmune disease.
Health care providers also consider CIDP as the chronic form of Guillain-Barré syndrome.
The specific triggers of CIDP vary. In many cases, the cause cannot be identified.
CIDP may occur with other conditions, such as:
- Chronic hepatitis
- Diabetes
- Infection with the bacterium Campylobacter jejuni
- HIV/AIDS
- Immune system disorders due to cancer
- Inflammatory bowel disease
- Systemic lupus erythematosus
- Cancer of the lymph system
- Overactive thyroid
- Side effects of medicines to treat cancer or HIV
Symptoms
Symptoms include any of the following:
- Problems walking due to weakness or lack of feeling in the feet
- Trouble using the arms and hands or legs and feet due to weakness
- Sensation changes, such as numbness or decreased sensation, pain, burning, tingling, or other abnormal sensations (usually affects the feet first, then the arms and hands)
Other symptoms that can occur with CIDP include:
- Abnormal or uncoordinated movement
- Problems breathing
- Fatigue
- Hoarseness or changing voice or slurred speech
Exams and Tests
The provider will perform a physical exam and ask about the symptoms, focusing on the nervous system and muscles.
Tests that may be ordered include:
- Electromyography (EMG) to check the muscles and the nerves that control the muscles
- Nerve conduction tests to check how fast electrical signals move through a nerve
- Nerve biopsy to remove a small piece of a nerve for examination
- Spinal tap (lumbar puncture) to check the fluid that surrounds the brain and spinal cord
- Blood tests may be done to look for specific proteins that are causing the immune attack on the nerves
- Lung function tests to check if breathing is affected
Depending on the suspected cause of CIDP, other tests, such as x-rays, imaging scans, and blood tests, may be done.
Treatment
The goal of treatment is to reverse the attack on the nerves. In some cases, nerves can heal and their function can be restored. In other cases, nerves are badly damaged and cannot heal, so treatment is aimed at preventing the disease from getting worse.
Which treatment is given depends on how severe the symptoms are, among other things. The most aggressive treatment is only given if you have difficulty walking, breathing, or if symptoms don't allow you to care for yourself or work.
Treatments may include:
- Corticosteroids to help reduce inflammation and relieve symptoms
- Other medicines that suppress the immune system (for some severe cases)
- Plasmapheresis or plasma exchange to remove antibodies from the blood
- Intravenous immune globulin (IVIg), which involves injecting antibodies into the bloodstream to reduce the effect of the antibodies that are causing the problem
Outlook (Prognosis)
The outcome varies. The disorder may continue long term, or you may have repeated episodes of symptoms. Complete recovery is possible, but permanent loss of nerve function is not uncommon.
Possible Complications
Complications of CIDP include:
- Pain
- Permanent decrease or loss of sensation in areas of the body
- Permanent weakness or paralysis in areas of the body
- Repeated or unnoticed injury to an area of the body
- Side effects of medicines used to treat the disorder
When to Contact a Medical Professional
Contact your provider if you have a loss of movement or sensation in any area of the body, especially if your symptoms get worse.
References
Katirji B. Disorders of peripheral nerves. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 106.
Smith AG, Shy ME. Peripheral neuropathies. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 388.
Review Date: 6/13/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.