Non-small cell lung cancer
Cancer - lung - non-small cell; Non-small cell lung cancer; NSCLC; Adenocarcinoma - lung; Squamous cell carcinoma - lung; Large cell carcinoma - lung
Non-small cell lung cancer is the most common type of lung cancer. It usually grows and spreads more slowly than small cell lung cancer.
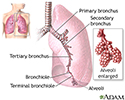
There are three common types of non-small cell lung cancer (NSCLC):
- Adenocarcinomas are often found in an outer area of the lung.
- Squamous cell carcinomas are usually found in the center of the lung next to an air tube (bronchus).
- Large cell carcinomas can occur in any part of the lung.
- There are other uncommon types of lung cancer that are also called non-small.
Causes
Lung cancer is the deadliest type of cancer for both men and women. Each year, more people die of lung cancer than of breast, colon, and prostate cancers combined.
Lung cancer is more common in older adults. It is rare in people under age 45.
Smoking causes most cases (around 80%) of non-small cell lung cancer. The risk depends on the number of cigarettes you smoke each day and for how long you have smoked. Being around the smoke from other people (secondhand smoke) also raises your risk of lung cancer. The risk decreases with time after you stop smoking. There is no evidence that smoking low-tar cigarettes lowers the risk. Some people who have never smoked do develop lung cancer.
Research shows that smoking marijuana may help cancer cells grow. But there is no direct link between smoking marijuana and developing lung cancer.
Constant exposure to high levels of air pollution and drinking water that has a high level of arsenic can increase your risk of lung cancer. A history of radiation therapy to the lungs can also increase risk.
Working with or living near cancer-causing chemicals or materials can also increase the risk of developing lung cancer. Such chemicals include:
- Arsenic
- Asbestos
- Radon
- Chemicals such as uranium, beryllium, vinyl chloride, nickel chromates, coal products, mustard gas, chloromethyl ethers, gasoline, and diesel exhaust
- Certain alloys, paints, pigments, and preservatives
- Products using chloride and formaldehyde
Symptoms
Symptoms may include:
- Chest pain
- Cough that does not go away
- Coughing up blood
- Fatigue
- Loss of appetite
- Losing weight without trying
- Shortness of breath
- Wheezing
Early lung cancer may not cause any symptoms.
Other symptoms that may be due to NSCLC, often in the late stages:
- Bone pain or tenderness
- Eyelid drooping
- Hoarseness or changing voice
- Joint pain
- Nail problems
- Shoulder pain or weakness
- Swallowing difficulty
- Swelling of the face
- Weakness
These symptoms can be due to other, less serious conditions. It is important to talk to your health care provider if you have symptoms.
Exams and Tests
Your provider will perform a physical exam and ask about your medical history. You will be asked if you smoke, and if so, how much you smoke and for how long you have smoked. You will also be asked about other things that may have put you at risk of lung cancer, such as exposure to certain chemicals.
When listening to your chest with a stethoscope, your provider may hear fluid around your lungs. This may suggest cancer.
Tests that may be done to diagnose lung cancer or to see if it has spread include:
- Bone scan
- Chest x-ray
- Complete blood count (CBC)
- Comprehensive metabolic panel
- CT scan of the chest and abdomen
- MRI of the chest
- Positron emission tomography (PET) scan
- Sputum test to look for cancer cells
- Thoracentesis (sampling of fluid buildup around the lung)
In most cases, a piece of tissue is removed from your lungs for examination under a microscope. This is called a biopsy. There are several ways to do this:
- Bronchoscopy combined with biopsy
- CT-scan-directed needle biopsy
- Endoscopic bronchoscopy ultrasound (EBUS) with biopsy
- Mediastinoscopy with biopsy
- Open lung biopsy
- Pleural biopsy
If the biopsy shows cancer, it may be checked for certain genetic changes that may lead to specific treatment. More imaging tests are done to find out the stage of the cancer. Stage means how big the tumor is and how far it has spread. NSCLC is divided into 5 stages:
- Stage 0 -- The cancer has not spread beyond the inner lining of the lung.
- Stage I -- The cancer is small and has not spread to the lymph nodes.
- Stage II -- The cancer has spread to some lymph nodes near the original tumor.
- Stage III -- The cancer has spread to nearby tissue or to far away lymph nodes.
- Stage IV -- The cancer has spread to other organs of the body, such as the other lung, brain, or liver.
Treatment
There are many different types of treatment for NSCLC. Treatment depends on the stage of the cancer and whether the cancer cells have genetic changes that create target molecules in or on the cells.
Surgery is the common treatment for NSCLC that has not spread beyond nearby lymph nodes. The surgeon may remove:
- One of the lobes of the lung (lobectomy)
- Only a small part of the lung (wedge or segment removal)
- The entire lung (pneumonectomy)
Some people need chemotherapy. Chemotherapy uses medicines to kill cancer cells and stop new cells from growing. Treatment may be done in the following ways:
- Chemotherapy is often used when the cancer has spread outside the lung (stage IV).
- It may also be given before surgery. This is called neoadjuvant therapy.
- It may be given after surgery to kill any remaining cancer. This is called adjuvant therapy.
- Chemotherapy is usually given through a vein (by IV).
Controlling symptoms and preventing complications during and after chemotherapy is an important part of care.
Immunotherapy can be given by itself or with chemotherapy.
Targeted therapy may be used to treat NSCLC. Targeted therapy uses medicines to zero in on specific target molecules in or on cancer cells. These targets play a role in how cancer cells grow and survive. Using these targets, the medicine disables the cancer cells so they cannot spread.
Radiation therapy can be used with chemotherapy if surgery is not possible. Radiation therapy uses powerful x-rays or other forms of radiation to kill cancer cells. Radiation may be used to:
- Treat the cancer, sometimes along with chemotherapy, if surgery is not possible
- Help relieve symptoms caused by the cancer, such as breathing problems and swelling
- Help relieve cancer pain when the cancer has spread to the bones
Controlling symptoms during and after radiation to the chest is an important part of care.
The following treatments are mostly used to relieve symptoms caused by NSCLC:
- Laser therapy -- A small beam of light burns and kills cancer cells.
- Photodynamic therapy -- Uses a light to activate a medicine in the body, which then kills cancer cells.
Support Groups
You can ease the stress of illness by joining a support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
The outlook varies. Most often, NSCLC grows slowly. In some cases, it can grow and spread quickly and cause rapid death. The cancer may spread to other parts of the body, including the bone, liver, small intestine, and brain.
Chemotherapy, immunotherapy, and targeted therapy have been shown to prolong life and improve the quality of life in some people with stage IV NSCLC.
Cure rates are related to the stage of disease and whether you are able to have surgery.
- Stage I and II cancers have the highest survival and cure rates.
- Stage III cancer can be cured in some cases.
- Stage IV cancer is almost never cured. The goals of therapy are to extend and improve the quality of life.
When to Contact a Medical Professional
Contact your provider if you have symptoms of lung cancer, particularly if you smoke.
Prevention
If you smoke, now is the time to quit. If you are having trouble quitting, talk with your provider. There are many methods to help you quit, from support groups to prescription medicines. Also, try to avoid secondhand smoke.
If you are age 50 to 80 years and have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years, ask your provider about being screened for lung cancer by low-dose CT scan of your chest.
References
American Cancer Society website. Lung cancer risk factors. www.cancer.org/cancer/types/lung-cancer/causes-risks-prevention/risk-factors.html. Updated January 29, 2024. Accessed June 3, 2024.
American Lung Association website. Lung cancer trends brief. www.lung.org/research/trends-in-lung-disease/lung-cancer-trends-brief. Accessed June 3, 2024.
Araujo LH, Horn L, Merritt RE, Shilo K, Xu-Welliver M, Carbone DP. Cancer of the lung: non-small cell lung cancer and small cell lung cancer. In: Niederhuber JE, Armitage JO, Kastan MB, Doroshow JH, Tepper JE, eds. Abeloff's Clinical Oncology. 6th ed. Philadelphia, PA: Elsevier; 2020:chap 69.
Centers for Disease Control and Prevention website. Health problems caused by secondhand smoke. www.cdc.gov/tobacco/secondhand-smoke/health.html. Updated May 15, 2024. Accessed June 3, 2024.
National Cancer Institute website. Non-small cell lung cancer treatment (PDQ) - health professional version. www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq. Updated March 8, 2024. Accessed June 3, 2024.
NCCN clinical practice guidelines in oncology: non-small cell lung cancer, version 6.2024. www.nccn.org/guidelines/guidelines-detail?category=1&id=1450. Accessed June 18, 2024.
Rivera MP, Mody GN, Weiner AA. Lung cancer: treatment. In: Broaddus VC, Ernst JD, King TE et al, eds. Murray and Nadel's Textbook of Respiratory Medicine. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 77.
US Preventive Services Task Force website. Final recommendation statement. Lung cancer: screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening. Updated March 9, 2021. Accessed June 3, 2024.
Lung cancer
Animation
Lungs - illustration
Lungs
illustration
Secondhand smoke and lung cancer - illustration
Secondhand smoke and lung cancer
illustration
Review Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.