Hemolytic anemia
Anemia - hemolytic
Anemia is a condition in which the body does not have enough healthy red blood cells. Red blood cells provide oxygen to body tissues.
Normally, red blood cells last for about 120 days in the body. In people with hemolytic anemia, red blood cells in the blood are destroyed earlier than normal.
Causes
The bone marrow is mostly responsible for making new red cells. Bone marrow is the soft tissue in the center of bones that helps form all blood cells.
Hemolytic anemia occurs when the bone marrow isn't making enough red cells to replace the ones that are being destroyed.
There are several possible causes of hemolytic anemia. Red blood cells may be destroyed due to:
- An autoimmune problem in which the immune system mistakenly sees your own red blood cells as foreign substances and destroys them
- Genetic variations within the red cells (such as sickle cell anemia, thalassemia, and G6PD deficiency)
- Exposure to certain chemicals, medicines, and toxins
- Infections
- Blood clots in small blood vessels
- Transfusion of blood from a donor with a blood type that does not match yours
- Faulty, damaged, or artificial heart valves
Symptoms
You may not have symptoms if the anemia is mild. If the problem develops slowly, the first symptoms may be:
- Feeling weak or tired more often than usual, or with exercise
- Feelings that your heart is pounding or racing
- Headaches
- Problems concentrating or thinking
If the anemia gets worse, symptoms may include:
- Lightheadedness when you stand up
- Pale skin
- Shortness of breath
- Sore tongue
- Left upper abdominal pain due to an enlarged spleen
Exams and Tests
A test called a complete blood count (CBC) can help diagnose anemia and offer some hints to the type and cause of the problem. Important parts of the CBC include red blood cell count (RBC), hemoglobin, and hematocrit (HCT).
These tests can identify the type of hemolytic anemia:
- Absolute reticulocyte count
- Coombs test, direct and indirect
- Donath-Landsteiner test
- Cold agglutinins
- Free hemoglobin in the serum or urine
- Platelet count
- Protein electrophoresis - serum
- Serum immunofixation
- Pyruvate kinase
- Serum haptoglobin levels
- Serum LDH
- Carboxyhemoglobin level
Treatment
Treatment depends on the type and cause of the hemolytic anemia:
- In emergencies, a blood transfusion may be needed.
- For immune causes, medicines that suppress the immune system may be used.
- When blood cells are being destroyed at a fast pace, the body may need extra folic acid and iron supplements to replace what is being lost.
In rare cases, surgery is needed to take out the spleen. This is because the spleen acts as a filter that removes abnormal cells from the blood.
Outlook (Prognosis)
The outcome depends on the type and cause of hemolytic anemia. Severe anemia can make heart disease, lung disease, or cerebrovascular disease worse.
When to Contact a Medical Professional
Contact your health care provider if you develop symptoms of hemolytic anemia.
References
Araten DJ, Brodsky RA. Paroxysmal nocturnal hemoglobinuria. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 32.
Gallagher PG. Hemolytic anemias: red blood cell membrane and metabolic defects. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 147.
Kumar V, Abbas AK, Aster JC, Deyrup AT, Das A. Hematopoietic and lymphoid systems. In: Kumar V, Abbas AK, Aster JC, Deyrup AT, Das A, eds. Robbins and Kumar Basic Pathology. 11th ed. Philadelphia, PA: Elsevier; 2023:chap 10.
Mentzer WC, Schrier SL. Extrinsic nonimmune hemolytic anemia. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 48.
Michel M, Jäger U. Autoimmune hemolytic anemia. In: Hoffman R, Benz EJ, Silberstein LE, et al, eds. Hematology: Basic Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 47.
Anemia
Animation
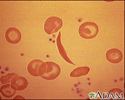
Red blood cells, sickle cell - illustration
Red blood cells, sickle cell
illustration
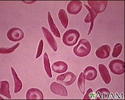
Red blood cells - multiple sickle cells - illustration
Red blood cells - multiple sickle cells
illustration
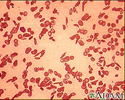
Red blood cells - sickle cells - illustration
Red blood cells - sickle cells
illustration
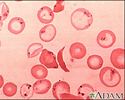
Red blood cells - sickle and Pappenheimer - illustration
Red blood cells - sickle and Pappenheimer
illustration
Blood cells - illustration
Blood cells
illustration
Red blood cells, sickle cell - illustration
Red blood cells, sickle cell
illustration
Red blood cells - multiple sickle cells - illustration
Red blood cells - multiple sickle cells
illustration
Red blood cells - sickle cells - illustration
Red blood cells - sickle cells
illustration
Red blood cells - sickle and Pappenheimer - illustration
Red blood cells - sickle and Pappenheimer
illustration
Blood cells - illustration
Blood cells
illustration
Review Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.